A 59-year-old woman presented to the Emergency Department with abdominal pain.
The pain was located in the epigastric area and right upper quadrant.
Vital signs were taken:
HR: 88bpm
BP: 164/99
RR: 24/min
95% on room air
Temp: 97.4F
The patient was seen by a PA.
An ultrasound and lab work were ordered. The labs showed a slight leukocytosis, lipase 415, and no evidence of urinary infection.
The ultrasound showed no evidence for gallstones or biliary dilatation.
The PA ordered a CT scan, but it was cancelled several minutes later.
The patient was given fluids, Zofran and several doses of morphine.
On reassessment her pain had improved from 10/10 to 5/10.
After consulting with the supervising physician, the PA discharged the patient home with hydrocodone/acetaminophen, ondansetron and famotidine.
Less than 24 hours later, the patient was going to the bathroom and suddenly felt dizzy.
She collapsed and was unresponsive.
Her family called 911, and EMS personnel started CPR and ROSC was achieved.
Tragically, she passed away a few hours after ICU admission.
Join 6300+ doctors and attorneys on the MedMalReviewer email list.
An autopsy was done on the patient, showing a gastric perforation and extensive amounts of foreign material in the peritoneal cavity.
The patient’s family contacted an attorney and a lawsuit was filed.
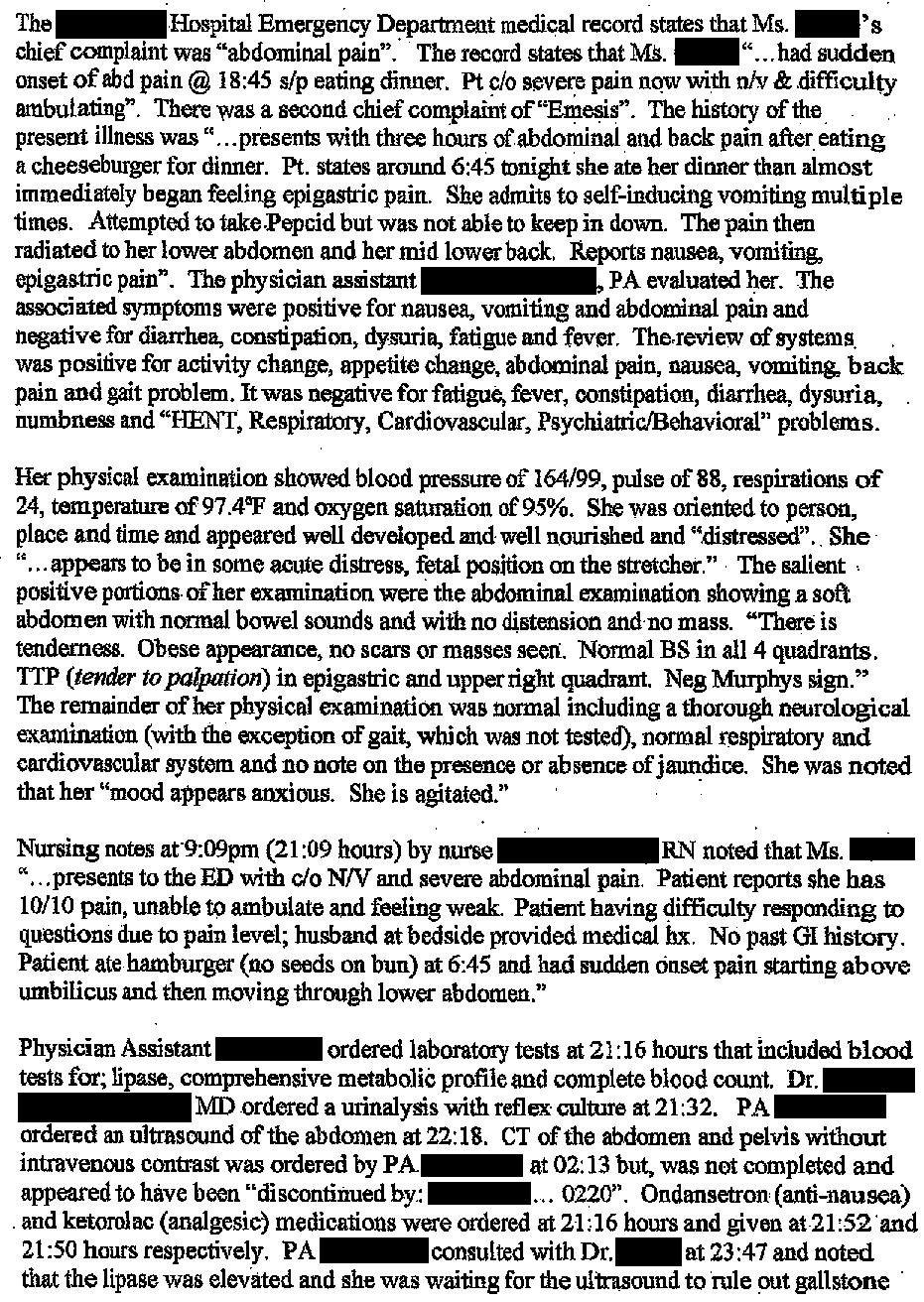
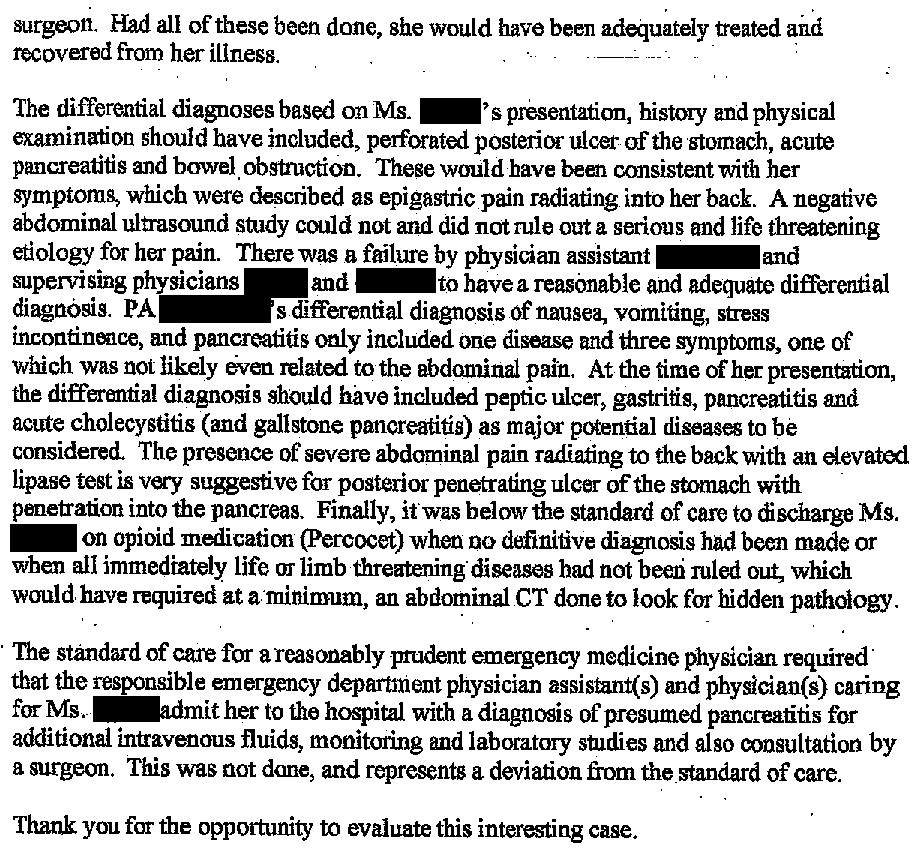
The expert witness opinion is shown here:
The patient’s estate offered to settle for $3.5 million.
The patient’s husband offered to settle for $500,000.
A confidential settlement was reached shortly before trial.
Free to sign up.
Paid options available for those who want to deepen their understanding.
MedMalReviewer Analysis:
The most painful thing about this case is that they ordered the test (CT abd/pelvis) that would have saved her life, but cancelled it a few minutes later. Drastic changes in workup plan should be accompanied by a one sentence explanation in the chart.
The PA had direct on-site supervision by EM physicians. In fact, 2 different physicians had the opportunity to make the diagnosis and both missed it. It does not appear that there was any miscommunication at sign-out that led to this bad outcome.
I suspect that the clinicians were suspicious of biliary disease based on the fact that she had RUQ pain immediately after eating a hamburger. In that context, it makes sense to order the ultrasound first. However, this case is a classic illustration of a few key principles in Emergency Medicine:
The need to focus the workup on the most worrisome differential diagnosis, rather than the most likely diagnosis.
The importance of re-directing the workup if the tests did not show the diagnosis you expected.
Resisting the urge to discharge patients just because they’ve already been in the ED for several hours.
Leave your comments at the link:
Become a medicolegal expert.
Improve your clinical acumen by reviewing a wide range of malpractice cases.
Pick up a subscription today to get a new case every week.
Previous Cases:
Hepatic Duct Injury [Subscribers Only]
Specialty: General Surgery
Synopsis: Hepatic ducts transected during cholecystectomy, Roux-en-Y attempted with poor anastomosis results, patient suffers numerous complications.
Doctor vs. Doctor Malpractice [Subscribers Only]
Specialty: Urology
Synopsis: A patient (who is a gastroenterologist) underwent surgery for prostate cancer, developing numerous abscesses, pelvic osteomyelitis, and cutaneous fistulas.
Specialty: OBGYN
Synopsis: A mother gives birth to a child with cystic fibrosis despite being told she was not at risk. Review of the case shows that the obstetrician never ordered the appropriate carrier screening.