A 48-year-old man (Mr. A) was found unresponsive in his yard at 7:00pm.
He had been seen normal between 6:00pm and 6:30pm.
He was rushed to a nearby hospital and underwent a workup including labs, CT head without contrast, and an MRI of his brain.
He was ultimately diagnosed with a stroke and given tPA nearly 4.5 hours after the stroke began.
He survived but with permanent disability.
The family sued the ED physician (Dr. Z) for not acting quicker.
They sued the neurologist for the same.
They also sued the radiologists (attending and resident) who read the non-contrast CT of the head, alleging that an MCA clot was visible but not reported.
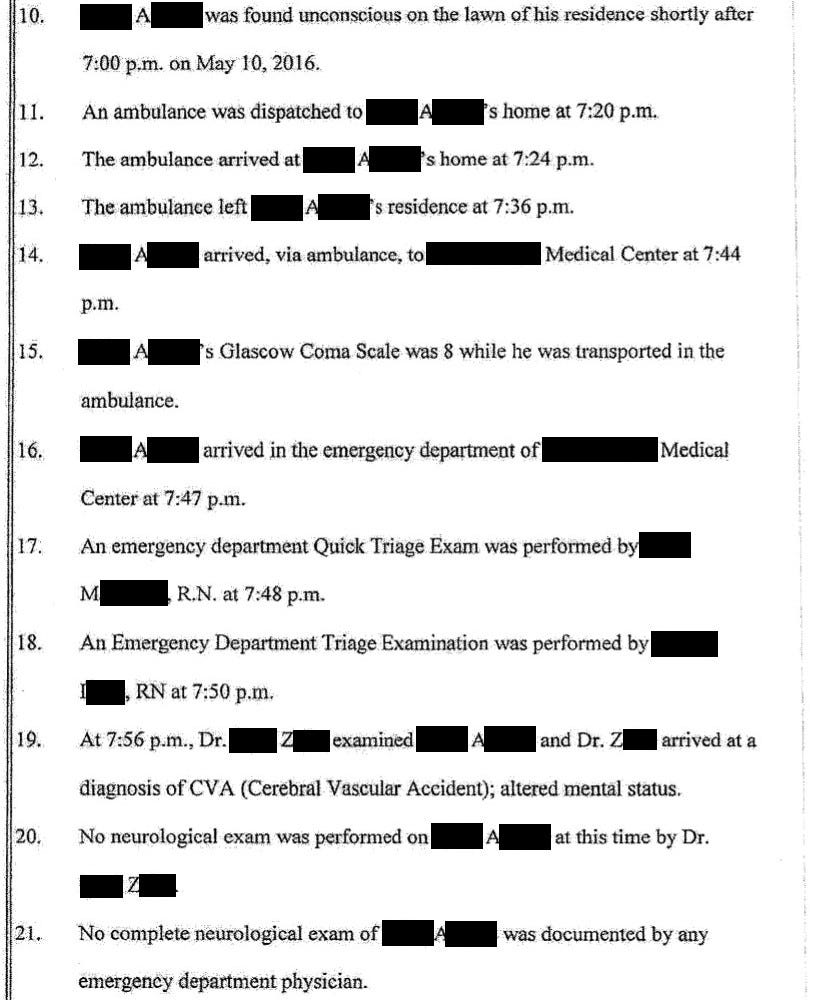
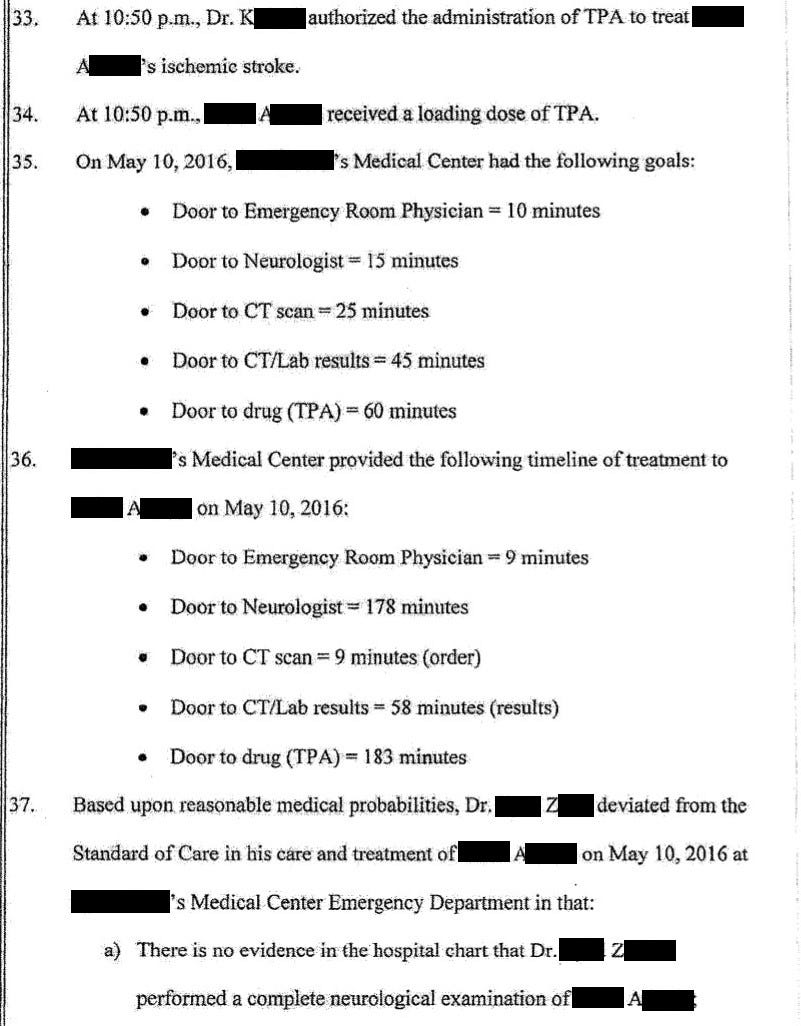
The plaintiff’s EM expert witness was dual-trained in EM/IM. This expert was hired because the ED physician was trained in IM but working in an ED.
Join 8000 doctors and attorneys on the email list.
The plaintiff also hired a neurologist.
The unique part of their opinion is shown here:
The plaintiff’s radiology expert wrote the following opinion:
2 years after the lawsuit was filed, the plaintiffs settled with the EM doctor.
On the same day, they offered to compromise with the neurologist and radiologist.
The defense attorneys for the radiologists and neurologist are now attempting to shift the blame to the ED doctor.
They’ve hired several ED physicians who have agreed to testify that this bad outcome was entirely his fault, not the radiologists or neurologist.
The defense vascular neurology expert is also arguing that giving tPA sooner would not have changed the outcome.
The plaintiffs accused the neurologist (Dr. K) of failing to transfer the patient to get thrombectomy done within 6 hours (standard of care in 2016).
The defense hired an expert who states this wasn’t possible.
The defense radiologist disagrees that there was a visible hyperdense MCA sign.
Final update:
The plaintiff ultimately settled with the neurologist and radiologist as well.
They were the last remaining defendants.
The lawsuit was withdrawn and no trial was held.
MedMalReviewer Opinion:
This lawsuit will bring up the perpetual debate about the risks/benefits of tPA. I have no interest in rehashing this argument here. There are reasonable doctors on both sides of the argument. It will be interesting to see if the defense attempts to bring this up and sway the jury.
From an ethical perspective, the radiology resident should not be a defendant in this case. Its wrong to blame trainees who are working under the direct supervision of an attending physician. From a legal and financial perspective, it provides the plaintiffs another target from which to extract a settlement.
The standard of care has changed between when this case occurred (2016) and when the lawsuit will be decided. Many institutions are now doing thrombectomy up to 24 hours after onset of symptoms. It is important for experts to opine about the standard of care when the case happened, not about current practice.
It does not appear that the ED physician ordered a stroke activation. This likely would have expedited every step of the process. He was likely thrown off by the fact that the patient didn’t have a classic “unilateral weakness” presentation. Its important to keep a stroke on the differential for patients who suddenly become unresponsive.
If you want to read more cases, subscribe to the newsletter to get a new case each week!
Become an expert; all the best cases and discussion are sent to paying subscribers.







He had an MRI result with 2.5 hours of arrival at the ED?! This is really impressively quick even for a large stroke center. These plaintiff experts must be high when they review these cases; they are clearly divorced from reality. This was a case of bad luck for the patient and not bad medical care. They got good care and those doctors were punished despite that.
The time from door to order and door to final report (for CT scan) misses a huge component. When the order is placed, The order has to be received by the radiology technician in the CT scanner, the patient has to be transported to the CT scanner, patient information his to be placed in the radiology information system(RIS). Patient has to be placed in the scanner, images have to be acquired and sent to the PACS (radiology images are a separate system from RIS) system in their entirety (can be 200 images for non contrast head CT up to 3000 for a ct angiogram of head. The images are then interpreted by radiologist. So when goal is 45 min door to CT read, it assumes a lot of things that radiologist has no control over. Their clock should not start until the images are fully acquired and sent to PACS.