This case concerns a 24-year-old woman, Ms. C. She was in a vehicle with her boyfriend (Mr. D) who broke up with her as they were driving. She was intoxicated, made suicidal statements, and tried to jump out of the moving vehicle. Mr. D stopped the car, called 911, and Ms. S was taken to a nearby ED.
At the ED, they were seen by an EM physician (Dr. S). The patient was medically cleared and evaluated by a member of the psychiatry team. The patient stated that she was no longer suicidal, contracted for safety, and was discharged with a referral for outpatient resources.
5 hours after discharge she jumped in front of a vehicle on the interstate and died. Police determined that she died by suicide.
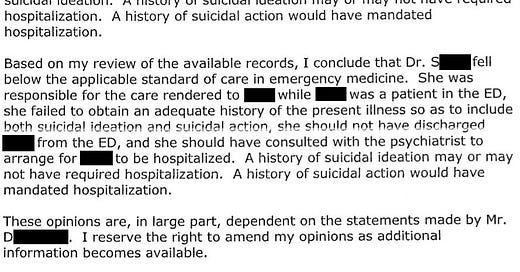
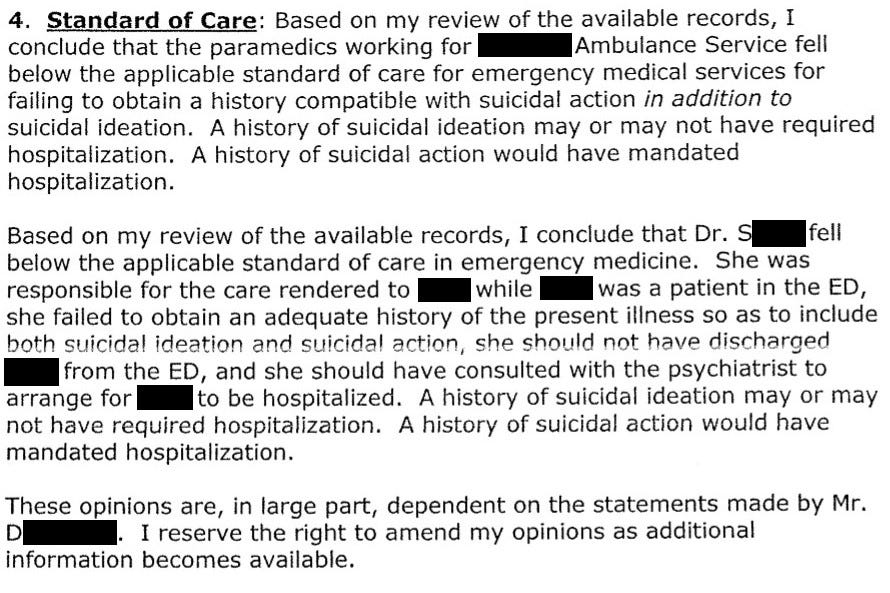
Her family filed a lawsuit against the EM physician, his employer, the social worker who did the in-depth psychiatric interview, the police officer who responded to the 911 call, and the ambulance service that transported her to the ED. In particular, the plaintiffs accused the EMS personnel of not communicating the fact that she tried to jump out of the moving vehicle to the ED physician.
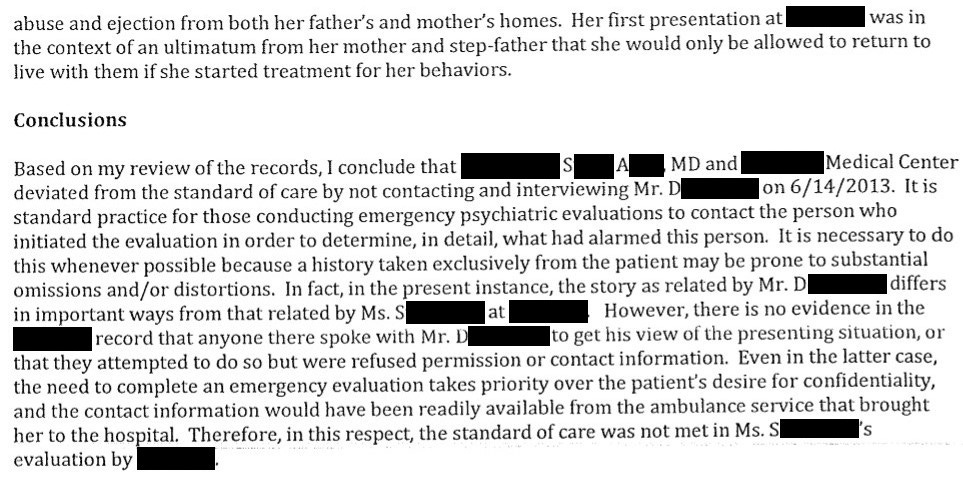
A psychiatrist was also hired as an expert witness. They were critical of the patient’s ED care, especially in regard to the fact that there was no documentation that collateral information was ever obtained from the patient’s boyfriend, who was with her when she attempted to jump from the vehicle.
Note that the patient went by several names, and here is referred to as Ms. S.
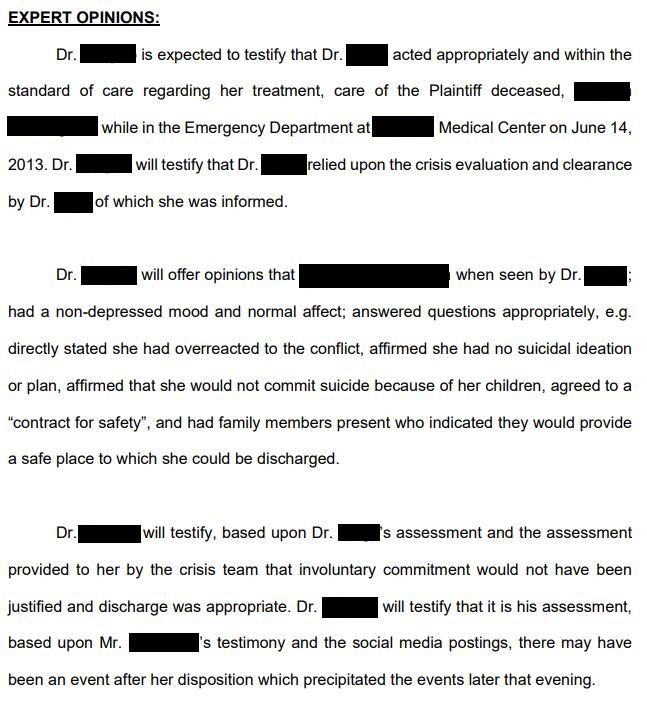
Later in the case, additional information came to light about the patient’s mental state after she was discharged. The patient’s ex-boyfriend reported that there was another disagreement after discharge that may have precipitated her suicide.
The defense hired an expert witness to review the case.
The defense expert felt that the discharge was appropriate, and that it was the events following discharge that likely played a key role in her death.
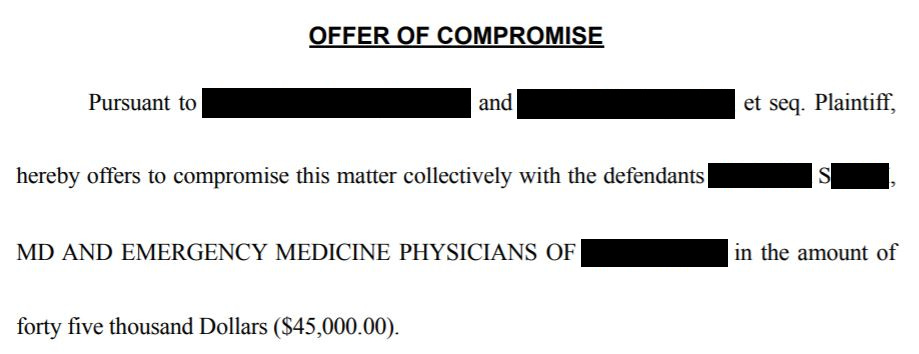
The plaintiff offered settlements to all defendants. The social worker was offered $475,000. The EM physician was offered $45,000.
All parties ultimately ended up settling for confidential amounts.
MedMalReviewer Opinion:
1) This was a very challenging case. The ED staff had multiple points of conflicting information. The patient was able to contract for safety, which is a pillar of safe discharge.
The nature of her statements prior to jumping out of the car also cloud the picture. “If you don’t let me out of this car I’m going to kill myself” seems to indicate how badly she wanted to get out of the car, less so that she was actively suicidal.
However, the ED physician documented the patient as saying “I’m going to kill myself”.
It was clearly difficult for the staff to determine where she was on the continuum from suicidal ideation to suicide plan to suicide attempt.
2) Collateral information is important. This applies especially in cases where a third party raised the concern, or if there is conflicting information on the patient’s psychiatric state. Talking to someone who knows the patient can provides useful information.
3) The relative size of the settlement offers to the ED physician and social worker are surprising. While I am not an expert on social worker malpractice insurance, I can’t imagine that the social worker carries a bigger policy than the physician.
Settlement offers usually reflect the size of the insurance policy. However, the settlement offers in this case may be more of an indicator of perceived culpability. Also keep in mind that a settlement offer does not necessarily tell us anything about the final amount of the (confidential) settlement.
EM physicians often rely on psychiatric screeners. They may be social workers, nurses, or have other training. In small hospitals, telepsychiatry may be used, or the ED physician may do the entire evaluation. This practice varies widely by hospital, with little standardization. When bad outcomes happen, the legal responsibility is often shared between all parties.
This is a high risk area for Emergency Medicine physicians and hospitals.
Recommended Reading
If you are interested in reading more about this topic, I highly recommend this blog post entitled “How to Write a Suicide Note” by The Last Psychiatrist.
It is written specifically for physicians seeing suicidal patients in the ED setting.
Want more cases?
Check out this recent case featuring an ischemic limb and compartment syndrome of a hand.
Read it here: Expert Witness Case #16 [Subscriber Content]



This is a fraught area. I think we (EM, society, patients, institutions, etc.) need to have a heart-to-heart about what is desired, where autonomy resides, where do I take away another person's right to do as they like with their body. This conversation will entail a lot of advocating and must include the assets to do what is requested. Telling EM physicians what they have to do then not giving them the resources (financial, legal, time, etc.) is not honest; current demands are childish (actions without responsibility.)
Very interesting here that there's no mention of the social worker or doctor diagnosing the patient with anything (e.g., bipolar, depressed, borderline personality, etc). Certainly, establishing the presence or absence of a major psychiatric diagnosis would be considered relevant to the assessment of safety vs. risk of suicide. A sad but very instructive case, thank you.