Expert Witness Case #32
This week’s case involves the care of a 60-year-old woman who presented to an ED with abdominal pain, nausea, and vomiting.
Her workup revealed DKA, and she was admitted to the hospitalist service on August 18. She was treated appropriately with fluids and IV insulin.
She was seen by the attending Dr. C, an intern Dr. A and senior resident Dr. C.
The next day (August 19), she developed 10/10 right leg pain with paresthesias in her toes. Her pain worsened throughout the day, she developed weakness, and the leg was cool to the touch.
Where else can you find unique malpractice cases with real-life exhibits?
Nowhere else.
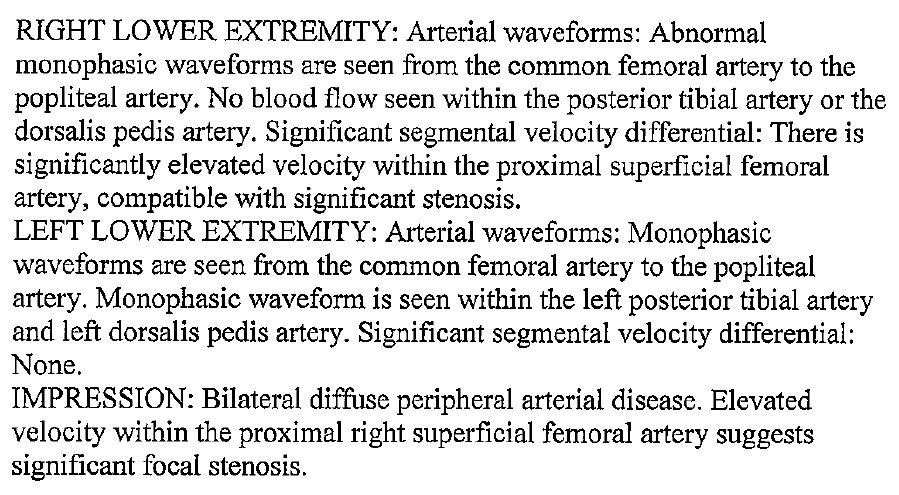
On August 20, an ultrasound was ordered. The results are shown here:
These results were reviewed by the resident and she documented a plan to “consider vascular consult given severe PAD results and significant stenosis”.
The next day a new attending (Dr. S) took over the hospital service. He noted black toes and inability to palpate a pulse in the right leg.
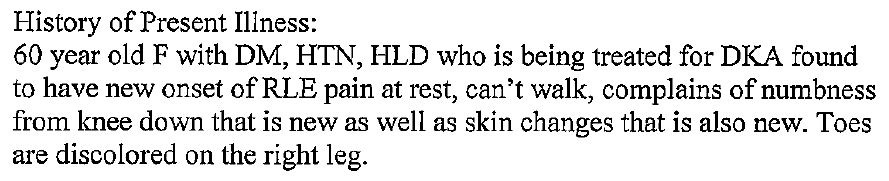
2 new residents also rotated onto the hospitalist service (Dr. B and Dr. M). They documented the following history and exam:
Given these findings, they ordered a CT angiography with run off, and discovered a large thrombus in the superficial artery and deep femoral artery.
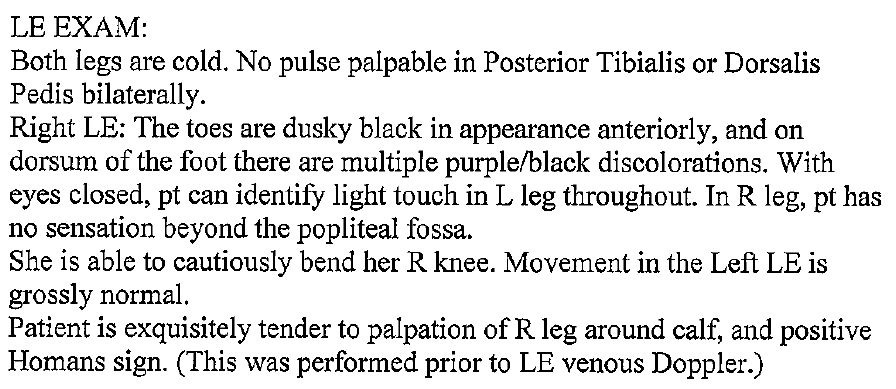
A vascular surgeon (Dr. B) was emergently consulted and wrote this note:
Dr. B performed a right femoral thrombendarterectomy and a four compartment fasciotomy. The next day her leg was amputated below the knee.
5 days later it was amputated above the knee.
The patient contacted an attorney, and a lawsuit was filed against all of the medicine attendings and residents, even those who came onto service and made the diagnosis.
The vascular surgeon was not sued.
An expert witness was hired who wrote the following opinion:
The lawsuit reached a confidential settlement.
Join 10,000+ doctors and lawyers who are improving their practice.
MedMalReviewer Opinion:
The case as presented by the plaintiff is quite damning. The patient had clear symptoms of arterial occlusion, which were not adequately addressed until several days later.
This case is a perfect illustration of how diagnostic momentum grinds to a snail’s pace once a patient is through the ED and on to an inpatient floor. The ED is accustomed to seeing acute ischemic limbs. Once you see it, you don’t forget the extreme pain. The ED also has processes in place to expedite their care, and is comfortable waking up a vascular surgeon in the middle of the night. There’s a significant chance the initial inpatient residents had never seen an ischemic leg before, and clearly were not equipped to correlate the ultrasound finding with the clinical exam. This is not a situation where you place an EMR order for a “formal” consult. You pick up the phone and ask the operator for the on-call vascular surgeon. There’s a big difference between formal consults and emergency consults, of which some inpatient doctors and consultants seem unaware.
The residents should have been dismissed from this lawsuit. The attending is responsible for all decisions made by the team, and must closely supervise their residents. Unfortunately the legal system simply does not view residents in this light, and in many states residents do not have any legal protections.
[Author’s note: I originally wrote this comment in December 2020, before they settled.] If I was providing risk management advice to the defendants or professional liability insurer, I would advise them to settle. The missed diagnosis is easy to understand from a layperson’s perspective, and the obvious and visible amputation will create a sympathetic jury.
Check out these previous cases:
Specialties: Critical Care, Hematology
Synopsis: A 37-year-old man with sickle cell disease presents with severe chest pain and hypoxia. Hematology consultant feels it is not acute chest syndrome and copy/pastes Up-To-Date as his consult note. Patient dies.
Specialty: General Surgery
Synopsis: A 58-year-old woman is diagnosed with cholecystitis in the ED. An injury to the common bile duct occurs during surgery. She survives with numerous complications.
Specialty: Emergency Medicine, Orthopedics
Synopsis: A 73-year-old woman has a knee replacement but goes to the ED with nausea and knee pain several days later. Discharged from the ED but at her next ortho appointment is diagnosed with a femur fracture.