A 51-year-old woman presented to an ophthalmology clinic with left eye discomfort.
She was diagnosed with keratitis, without a clear cause identified.
Over the next month she returned for multiple visits as her symptoms were not improving.
She was put on tobramycin and steroid eye drops.
She also visited an ER, where she was evaluated and referred back to the ophthalmology clinic.
It is clear from the documentation that her ophthalmologists had a differential of numerous potential causes but never arrived at a final diagnosis.
Eventually the ophthalmologists decided she either had HSV or acanthamoeba keratitis.
She was referred to an academic eye center.
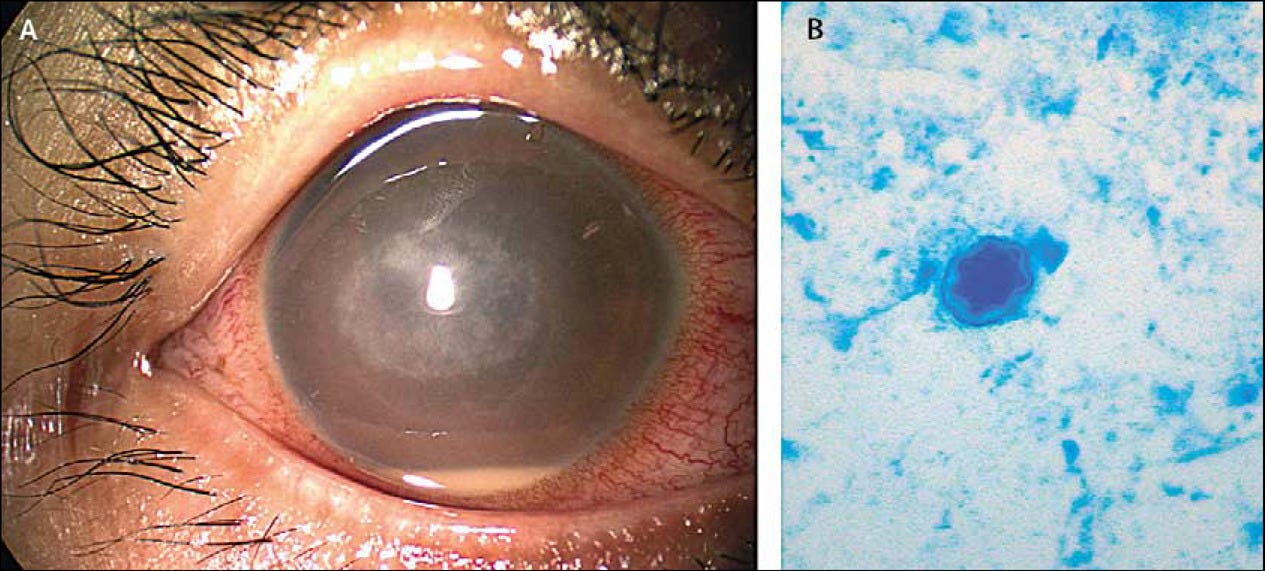
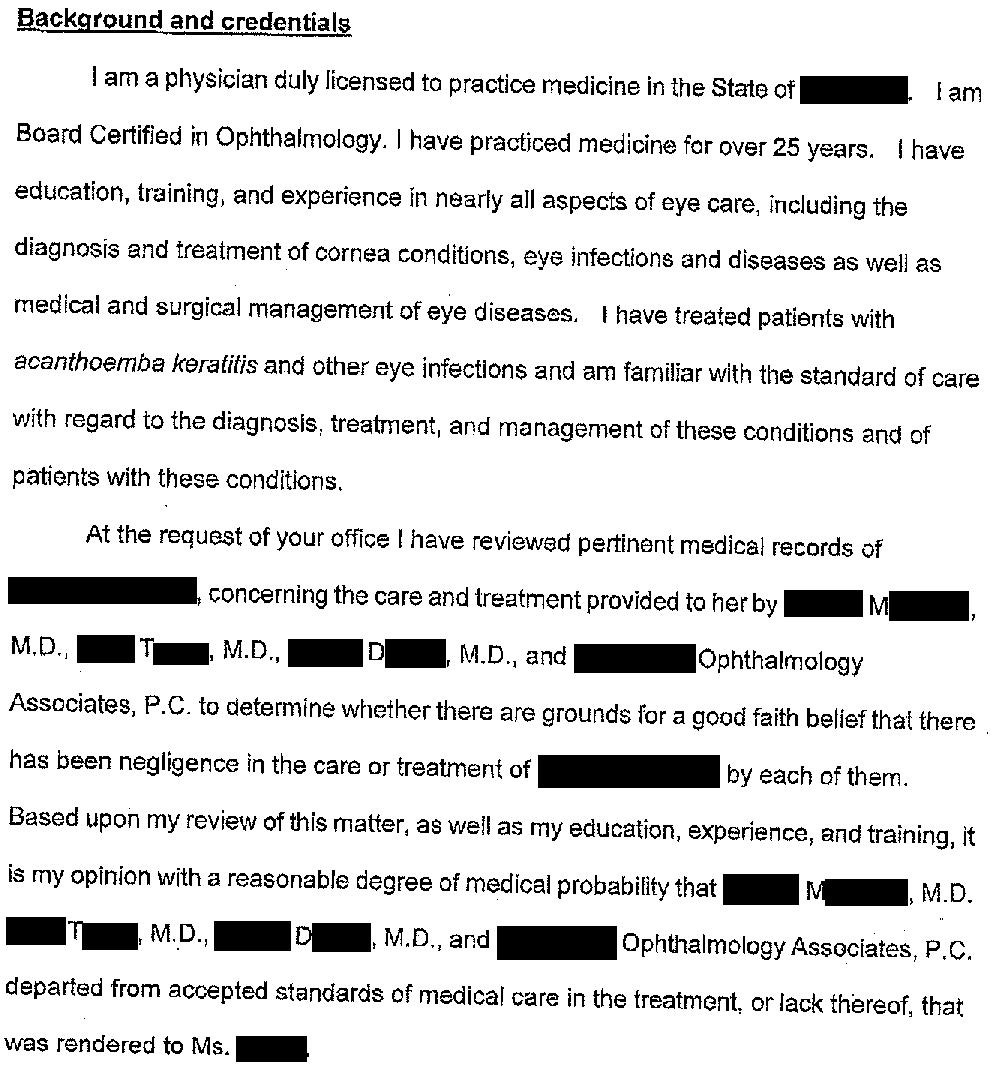
The diagnosis of acanthamoeba keratitis was confirmed.
Unfortunately she had permanent loss of vision in her left eye.
The patient was understandably upset about her loss of vision, and felt that the diagnosis took too long.
She contacted a malpractice attorney and a lawsuit was filed against the ophthalmology clinic and all 3 ophthalmologists who saw her.
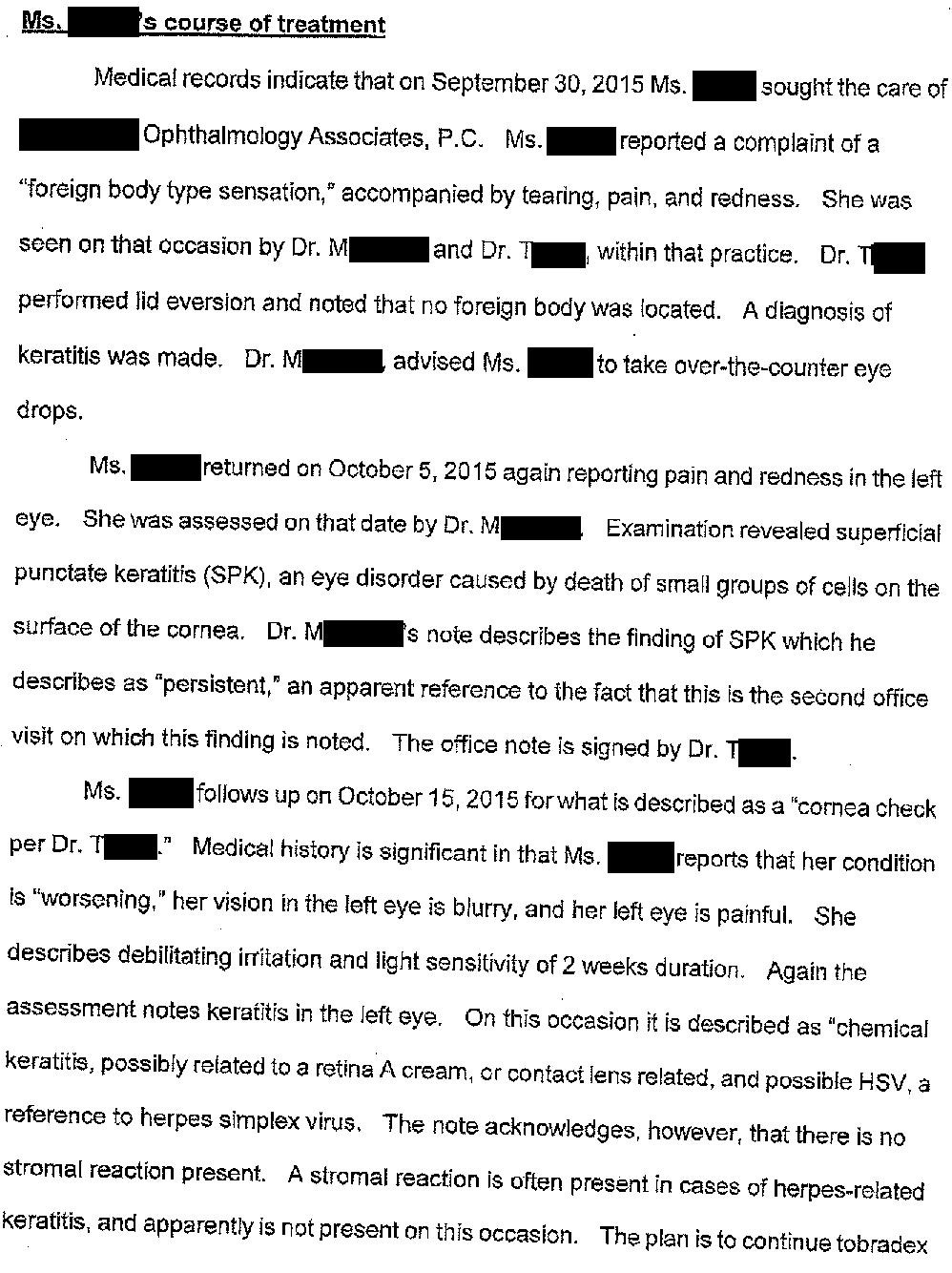
An expert witness was hired and wrote the opinion below.
Join 7100+ doctors on the email list.
Subscribe today to get a new case every week.
Grow your medicolegal expertise and learn from interesting malpractice lawsuits.
The lawsuit is still ongoing.
The plaintiff has indicated they are willing to settle the case.
A trial is scheduled for March 2022.
I’ll send email updates to subscribers as the lawsuit unfolds.
MedMalReviewer Analysis:
Acanthamoeba are a genus of amoeba that can cause both eye infections and brain infections. Note that this is a different genus of amoeba than the “brain-eating amoeba” that often get a lot of attention in the lay press, caused by Naegleria fowleri.
A broad differential is always important. Many of us are familiar with the fact that Pseudomonas is the most common cause of bacterial keratitis (especially in contact lens wearers) and are tempted to jump to this conclusion. It’s important to remember that there are numerous potential infectious causes of keratitis, and to pursue more aggressive diagnostics when a patient is not responding as anticipated.
A previous Acanthamoeba keratitis outbreak was discovered by the CDC (unrelated to this lawsuit) in 2007 after connecting a contact lens solution to numerous cases. PCR testing ultimately proved that the lens solution was the source of the Acanthamoeba.
As suggested by EyeWiki, the prognosis is poor and treatments are lengthy and toxic. I’m looking forward to hearing back from any ophthalmologists about their opinion on this case. Leave a comment or reply to this email!
The plaintiff is asking for a $1,000,000 settlement. Whether or not the ophthalmologists were truly negligent, I think it is probably wise to negotiate and settle this case. A delayed diagnosis resulting in loss of vision will find a very sympathetic jury.
Here’s a little bonus for the real nerds in the group…
Dr. Bobbi Pritt is a pathologist who runs a wonderful blog on parasitology.
She’s been publishing weekly cases for… 667 weeks! Creating good content for that long is truly impressive. This is only my 89th weekly case so I have a ways to go to catch up with her.
Here are some excellent real-life examples of what a pathologist may see when a patient is being evaluated for Acanthamoeba keratitis: Case 410, Case 542, Case 90.
Previous Cases:
Respiratory Arrest [Subscribers Only]
Ophthalmology takes patient to OR for planned surgery. Admitted to med/surg floor afterward, given Dilaudid, patient goes apneic and dies.
Family sues ophthalmology, anesthesia, and the hospitalist.
Patient presents to free-standing ED with a STEMI. Challenging intubation with severe hypoxia. Patient survives transport to cath lab but dies of cardiogenic shock.
Family sues the ER doctor.
EMS Compartment Syndrome [Subscribers Only]
Unresponsive diabetic given D50 by EMS. Infiltration occurs, compartment syndrome develops, patient suffers permanent arm dysfunction.
Patient sues the EMS company, wins $725,000 directed verdict.




polyhexamethylene biguanide -- it’s compound used for chlorine free pool water antiseptic... or something you poor onto your eyes for weeks hoping it keeps acanthamoeba
I agree that it is inexplicably negligent not to culture the infection once an infiltrate has appeared and is threatening vision or not responding to treatment. However in this case it being Acanthamoeba it likely did not truly change long term outcome. The best medical treatment is pool antiseptic which is off label, it’s not a very effective treatment, often transplants have to be done to try and cut out the infection but they often recur as it is horrendously difficult infection to treat.