Gastric Bypass Catastrophe
Case #225
A 32-year-old woman with a BMI of 45 was referred to a bariatric surgeon.
After consultation, she underwent a Roux-en-Y gastric bypass with Dr. Z.
Several months later she was taken back to the OR for abdominal pain.
Several adhesions were taken down.
About one year after the initial surgery, she was taken back for a revision.
During the first 2 postoperative days, she had extreme pain.
She developed hypotension, tachypnea, and hypoxia.
Repeat labs were done, showing a lactate of 8.8, and she was moved to the ICU.
Improve your practice by learning from malpractice lawsuits.
Paying subscribers get access to the entire archive.
In the ICU, an echo was done, and there was discussion about doing CT scans.
Nearly 12 hours after the lactate result, Dr. Z took her back to the OR.
She had a grossly contaminated abdomen full of feculent material, coming from the anastomosis site.
She was eventually transferred to another hospital in severe sepsis on 3 pressors.
Over the course of several weeks, she remained in fulminant organ failure.
She had full thickness necrosis of skin on her abdomen and flanks.
Facing no prospect of meaningful survival, and all 4 extremities that were completely ischemic and would require amputation, her family elected to switch to comfort care and let her die as peacefully as possible.
Her family consulted with a law firm that specialized in medical malpractice.
A lawsuit was filed against Dr. Z and the hospital.
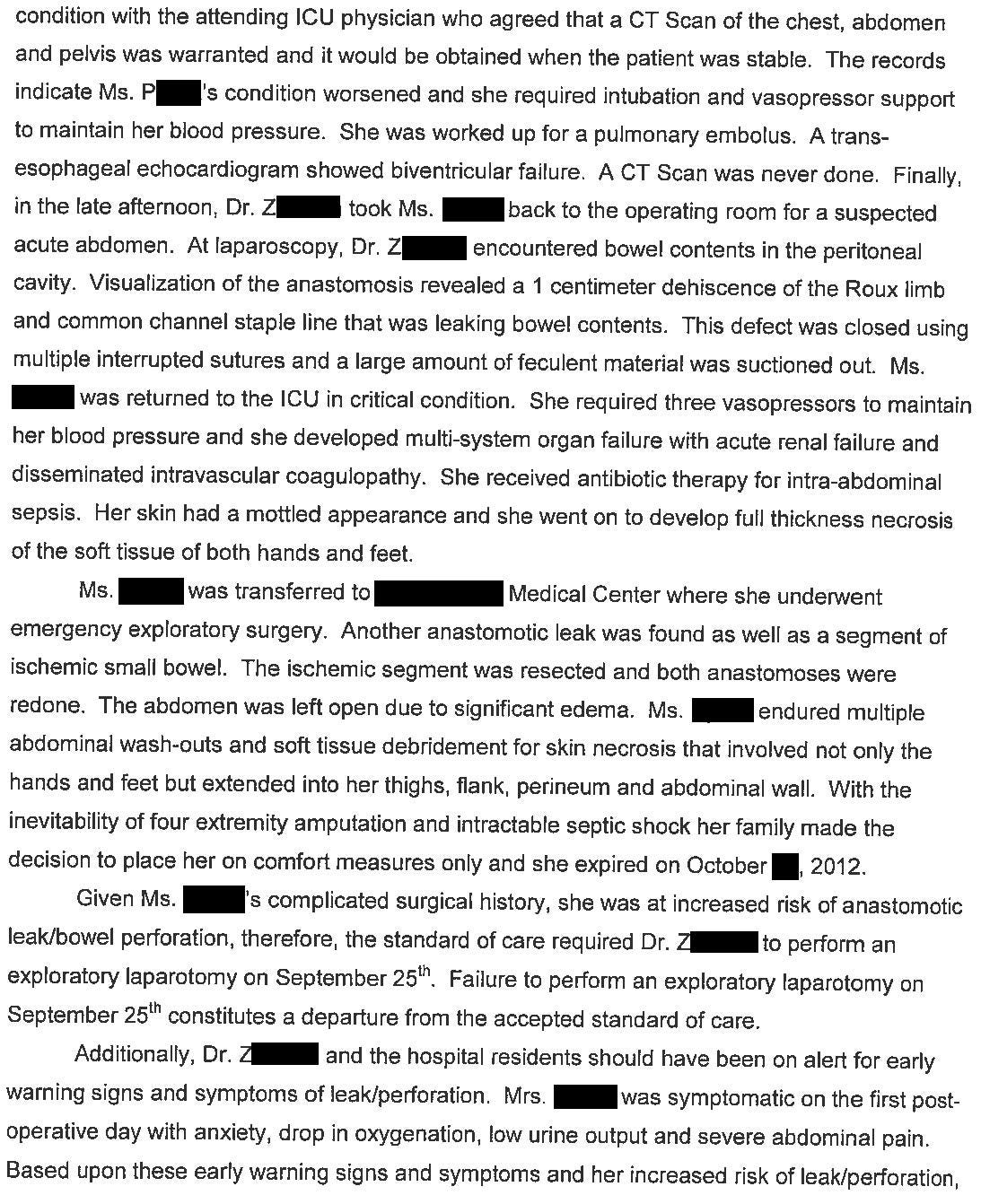
The expert witness opinion is shown here:
The plaintiff and the defendants reached a confidential settlement.
Become a medicolegal expert.
Paying subscribers get a new case every week.
MedMalReviewer Analysis:
The primary criticism was the delay in taking her back to the OR. Hindsight is 20/20, but there does seem to be some validity to the plaintiff’s allegations. I think the surgeon was desperately hoping for another cause of her shock with a lactate of >8, but unfortunately hope does not cure perforated bowel or a failed anastomosis causing abdominal sepsis. They reacted sluggishly in the face of a diagnosis that demanded decisive action.
The management of obesity has changed drastically since 2012. I am biased by only seeing the complications of these surgeries, but its hard to overlook the extremely awful outcomes for a small percentage of these patients, even if they’re rare. I haven’t seen any GLP-1 lawsuits yet, but I’m sure they’re coming.
I’ve published a few other related lawsuits (for paying subscribers):





This is like watching a car accident in slow motion. Pain attributed to “anxiety.” Pain out of proportion to exam. Sitting on a lactate of 8.8 for 12 hours. PE used as a scapegoat to the point of starting a heparin drip and NO scan. This is a great case for new ICU attendings to learn from.
I hate this idea that an emergent CT scan needs to wait for the pt to be more stable. Sometimes, they aren’t getting any more stable. Maybe a doctor even needs to accompany the pt to the scanner. But the scan needs to get done. In this case, it would have definitely made the diagnosis.