Mr. G was a 51-year-old man who presented to the ED with sudden onset of chest pain.
He had hypertension and diabetes.
There was no STEMI on his EKG.
His troponin was markedly elevated.
CT scan of his chest ruled out PE and dissection.
He was admitted to the ICU for NSTEMI and hypertensive crisis.
The next day he had a catheterization, revealing multi-vessel disease.
The hospital did not have a cardiothoracic surgeon.
The patient was transferred to another hospital about 10 miles away.
At the second hospital, he was seen by Dr. L, a cardiothoracic surgeon in private practice.
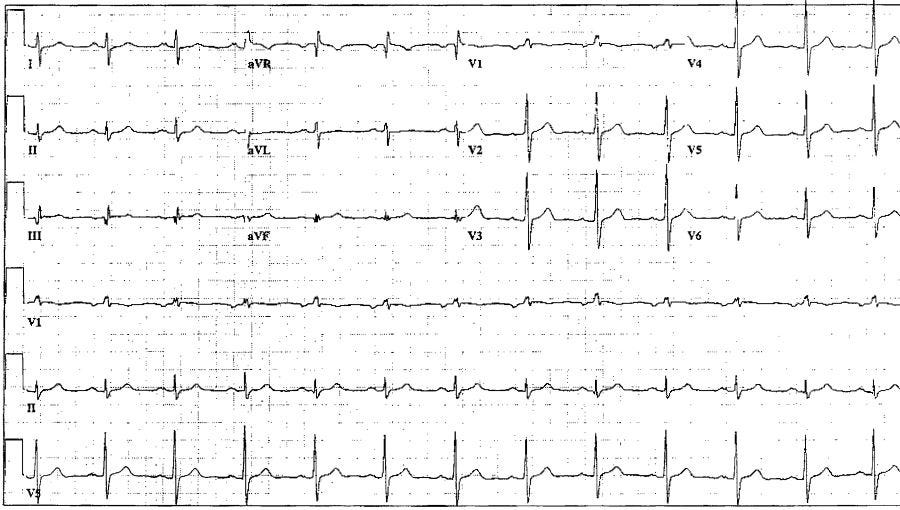
On arrival, Mr. G had no chest pain and his EKG is shown below:
Dr. L recommended a 4-vessel CABG.
The operation itself was uneventful.
Dr. L was assisted by Dr. P, a cardiothoracic surgeon employed by the hospital.
Dr. P was responsible for closing his chest.
He used 5 wires and 2 ZipFix ties.
Once the chest was closed, he was taken to the ICU.
Over the next few days, the ICU staff had difficulty weaning the vent.
He was frequently thrashing around, and sedation was difficult to manage.
The patient had persistent coughing spells.
On POD#4, he developed a fever.
ID was consulted and started vancomycin and Zosyn.
His agitation and delirium persisted as the ICU staff attempted to find an appropriate balance of sedation.
He had ongoing spells of hypoxia and ventilator dyssynchrony.
On POD#6, a CT of his chest was done:
Dr. L realized that the sternotomy had dehisced.
He documented that the wires had “pulled through” the sternum.
He was going on vacation for the next few days (Labor Day weekend).
He planned to repair the sternum after the weekend, hoping that the patient’s tenuous clinical status would improve.
He signed out to Dr. B, another cardiothoracic surgeon who was covering over the weekend.
When Dr. L left the hospital that Friday, it was the last time he would see the patient alive.
Dr. L would later testify that he told the ICU physicians to keep the patient sedated, and if necessary, to keep him paralyzed.
On Saturday the nursing notes documented “wild thrashing in bed”.
On Sunday (POD#10), his nurse decided to give him a sponge bath.
He had another severe coughing episode.
A nurse extender was in the room with him while the nurse was getting medication:
The nurse rushed into the room.
She attempted to use blankets to apply pressure to the massive hemorrhage.
The PA (Mr. S) described what he witnessed:
A strip from the code is shown below:
An autopsy was done the next day.
The relevant excerpt is shown below:
Join 9500 doctors and lawyers on the email list.
Free to join, paid options available for those who want a new case every week.
Dr. L was informed of what happened to the patient.
A meeting was held with the hospital staff and both Dr. L and Dr. B.
They were suspicious that the ZipFix ties had malfunctioned.
Dr. L sent the patient’s wife a letter, asking her to come to the office to discuss the situation.
He made a note about the discussion:
The patient’s wife contacted a law firm.
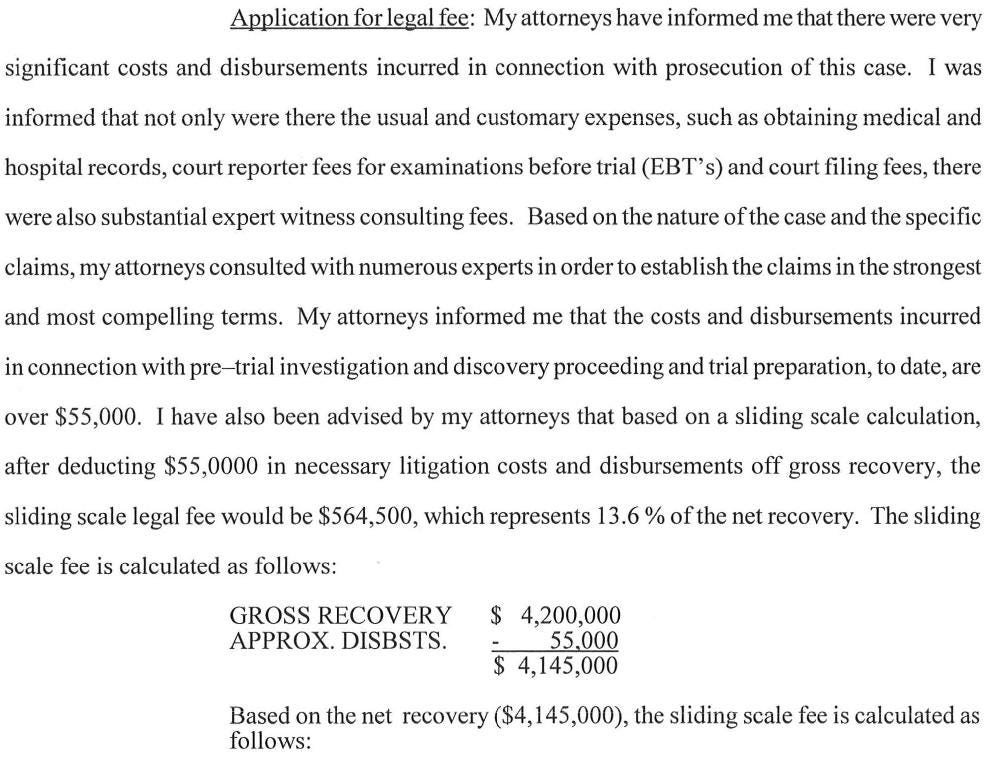
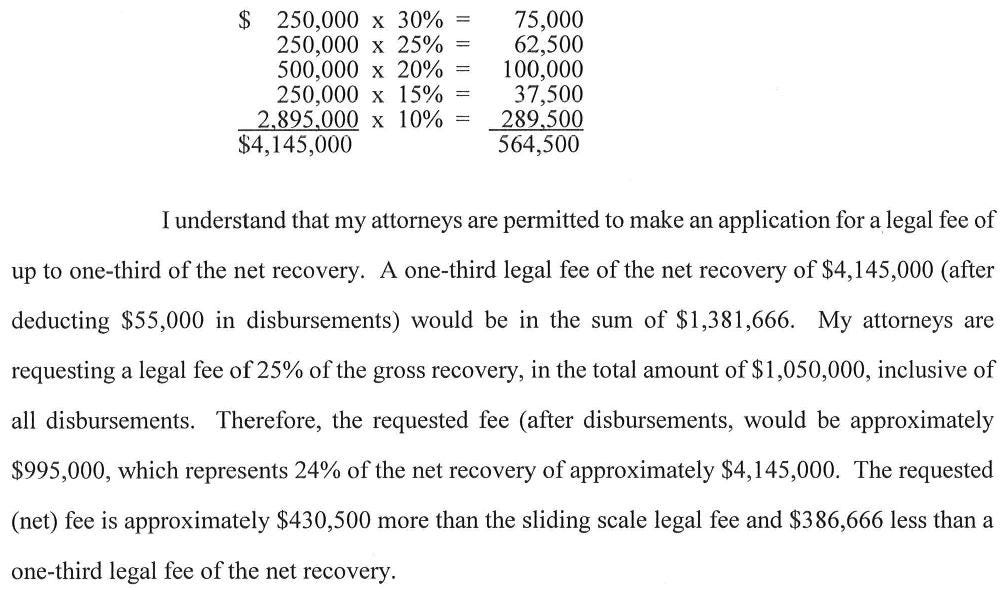
A retainer was signed that would pay the law firm up to 1/3 of the money recovered from a settlement or verdict.
They sued all 3 cardiothoracic surgeons, the ICU physician, their respective employers, and the hospital itself.
They also sued the company that made the ZipFix sternal closure device.
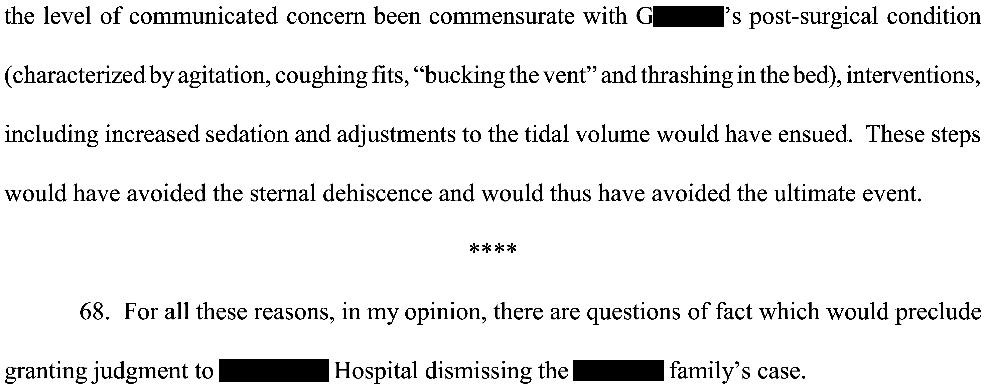
The hospital filed a Motion for Summary Judgment, in an attempt to be removed from the lawsuit.
The plaintiff opposed this motion, and disclosed their expert witness’ opinion.
He is a pulmonary/critical care physician with over 40 years of experience.
The hospital’s Motion for Summary Judgment was denied.
Settlement negotiations were held with each of the defendants.
The hospital settled for $200,000.
All 3 cardiothoracic surgeons settled together for $4,000,000.
The patient’s wife agreed to pay the attorneys $1,050,000 of this amount:
The judge authorized the legal fee of $1,050,000.
The plaintiff decided to voluntarily remove the ZipFix device manufacturer from the lawsuit, without a settlement.
The ICU doctor and his employer did not want to settle, as they felt that they were not responsible for the bad outcome.
The lawsuit took several years to move forward.
They took the case to trial, but agreed to a settlement before the jury reached a verdict.
The ICU doctor settled for $2,300,000.
The ICU doctor’s group settled for $1,200,000.
There were no court records to indicate how much the law firm made from this portion of the settlement.
MedMalReviewer Analysis:
This is the first lawsuit I’ve encountered that included the exact settlement amount (they’re usually confidential). I’m not clear if they forgot to redact this information or if this is standard procedure for this jurisdiction.
The contingency agreement shown here is actually lower than some I’ve seen. A flat fee of 33.3% is not uncommon.
The 7-figure payment to the law firm is significant, but keep in mind that the law firm had multiple partners and numerous staff members working on this case for 9 years.I’m not a cardiothoracic surgeon and don’t have any expertise with managing a sternal dehiscence. However, the plaintiffs do make a compelling argument that this should have been repaired earlier. The optics are particularly bad given that the surgeon was on vacation. It gave the plaintiff a narrative the he put greater importance on his vacation than on providing the appropriate care.
The plaintiff was able to turn the surgeon and the ICU doctor against each other. The surgeon accused the ICU of not keeping him properly sedated/paralyzed. The ICU doctor suggested that the surgeon should have taken him back sooner. Its never a good sign when the defendants are trying to blame each other.
If you like this case, please share it on Facebook!
Facebook blocked my publication, but this link still works and the case will be listed at the very top of the page: https://substack.com/profile/9224497-med-mal-reviewer












This is a crazy case. Thanks for sharing.
This is horrifying! The poor man was conscious with his heart outside of his chest and he was bleeding out. His family had to have been devastated. I know it would (if it was my dad) keep me awake for a very long time, and counseling would be required. What a terrible way to lose someone you loved, or even knew about. This convinces me, further, that everyone should have an advocate with them during a hospital stay, such as this had predicted for post-op.