We just hit a big milestone: 10,000 doctors and attorneys on the email list.
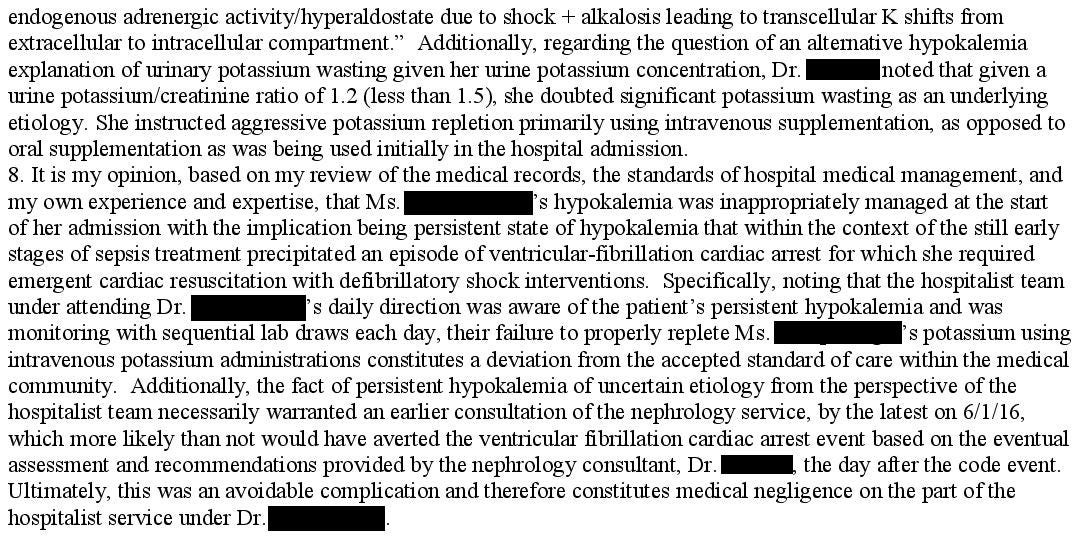
Thank you all for subscribing, it really means a lot to me.
A 64-year-old woman presented to the ED with left leg swelling and erythema.
She had a history of osteomyelitis, chronic leg wounds, hep C, and anal cancer.
Workup was worrisome for recurrent osteomyelitis.
She was started on IV antibiotics and admitted to the hospitalist.
A BMP showed a potassium of 2.6.
Over the next few days she received PO and IV potassium replacement.
Her potassium stayed between 2.5 and 2.8 despite replacement attempts.
An ID doctor was consulted due to recurrent osteomyelitis and history of both MRSA and pseudomonas infections.
A cardiologist was consulted for a TEE due to concern for endocarditis.
She had an EF of 55% and no vegetations were seen.
On hospital day #4, she suddenly went into cardiac arrest.
A code blue was called.
She was in V fib.
Fortunately, defibrillation was successful.
She was transferred to the ICU.
The patient survived with a good neurologic outcome.
One day before discharge, she had a repeat echo that showed an unchanged EF of 55%.
Several months later, she became ill again.
Blood cultures and another echo confirmed endocarditis.
She would ultimately undergo both aortic and mitral valve replacements.
The patient contacted a law firm.
She sued multiple physicians, alleging that she went into cardiac arrest because they mismanaged her hypokalemia.
The ER doctor, 2 hospitalists, the ID physician, and the cardiologist who did her TEE all were named as defendants.
They allege that she ultimately developed endocarditis and needed valve replacements because of the cardiac arrest.
The plaintiffs hired a heme/onc physician as an expert witness:
Expand your medicolegal expertise.
Paying subscribers get a new case every week, spanning numerous different specialties and legal issues.
The defense hired multiple experts, including a cardiologist (Dr. W):
It appears that the ED physician and ID physician were dismissed from the lawsuit.
Confidential settlements were reached with the hospitalists and cardiologist.
MedMalReviewer Analysis:
The arguments made by the plaintiff are weak at multiple points. While hypokalemia can certainly contribute to an arrhythmia, there were multiple other potential causes including sepsis. Her endocarditis was likely caused by the numerous episodes of osteomyelitis preceding this, not a cardiac arrest allegedly precipitated by hypokalemia.
The patient was represented by an attorney in a solo practice. I’m not a lawyer, but its obvious that he had no idea what he was doing. There were very basic lapses including failing to disclose experts that had the same training as the defendants. I’m guessing that numerous other competent law firms turned this case down. I was surprised to see that his website listed medical malpractice as one of his areas of expertise.
This lawsuit wasted the time of numerous physicians over the course of several years. Imagine the stress from having treated a patient appropriately, literally saving their life from the complications of their pre-existing medical condition, and then being sued by the patient. They should have received a thank-you note, not a summons. I hope the attorney lost a lot of money on this case and will be dissuaded from filing incredibly weak and poorly-litigated lawsuits in the future.
>100 EM docs searched for a job on www.attendingjobs.com last month.
Its the official jobs board of MedMalReviewer.
Let me know if you need to hire an EM doc, or need help finding a good job.




Am I missing something in this case, what was done wrong here? The patient was obviously very sick with many chronic illnesses, why did they reach settlements? A cardiac surgeon I worked with for a long time would always tell me it didn’t matter how well you treated a patient, they can always sue you and you would have to pay just to save time and make the problem go away. Is this really how it works? No wonder healthcare is so expensive in the US