Ms. O had a history of chronic abdominal pain and was seen by a gastroenterologist (Dr. W).
He was concerned she may have sphincter of Oddi dysfunction.
He recommended an ERCP, which was performed with the assistance of a CRNA (Mr. R) and a supervising anesthesiologist (Dr. A).
The legal documentation notes that during the procedure she was given both propofol and ketamine. These medications resulted in respiratory depression and the patient suffered a respiratory arrest with prolonged hypoxia.
The patient suffered a severe anoxic brain injury.
She died one month after the procedure.
Become a medicolegal expert.
Paying subscribers get a new case every week and access to the entire archive.
The patient’s family filed a lawsuit against the anesthesiologist, the gastroenterologist, and their respective employers.
Note that they did not sue the CRNA individually, but they did sue the anesthesia group that employed him.
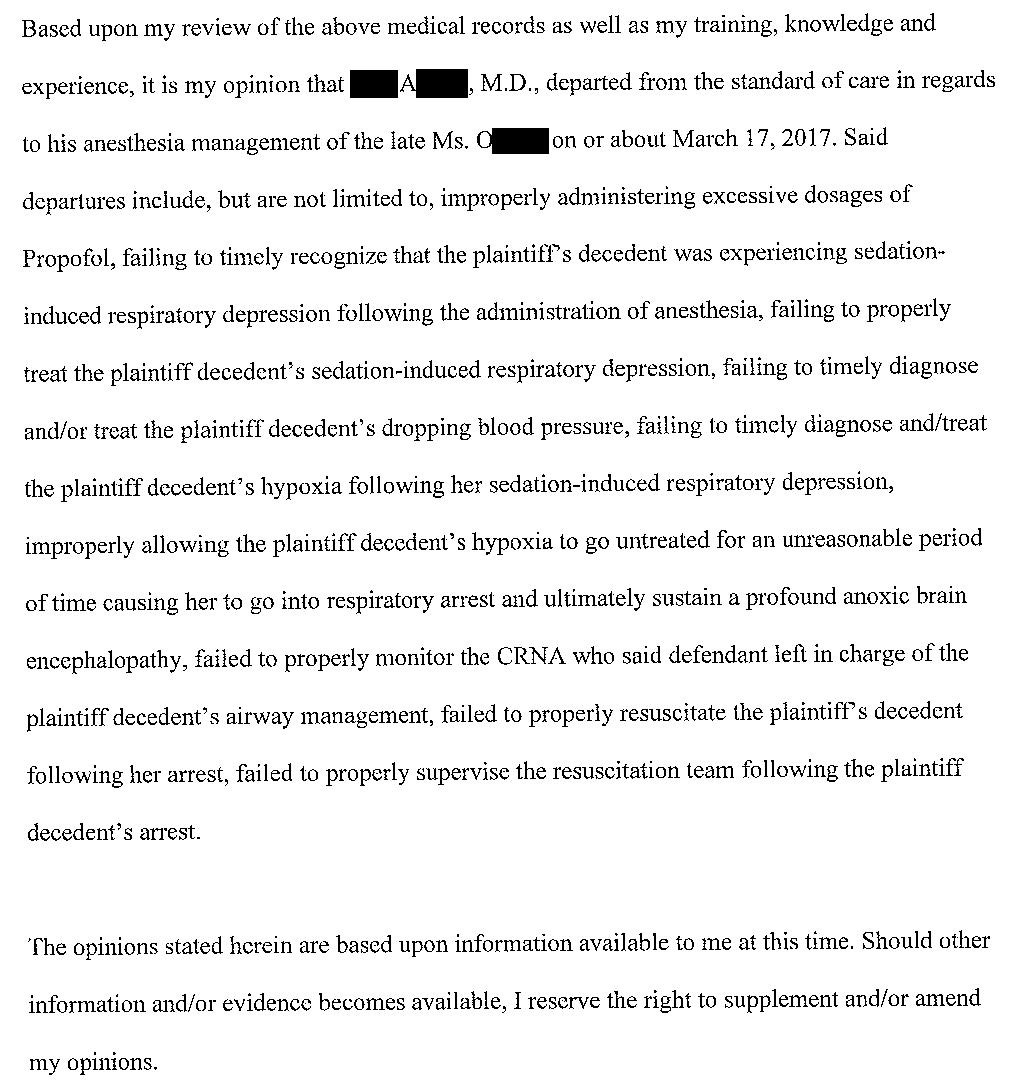
The anesthesiologist’s opinion is shown here:
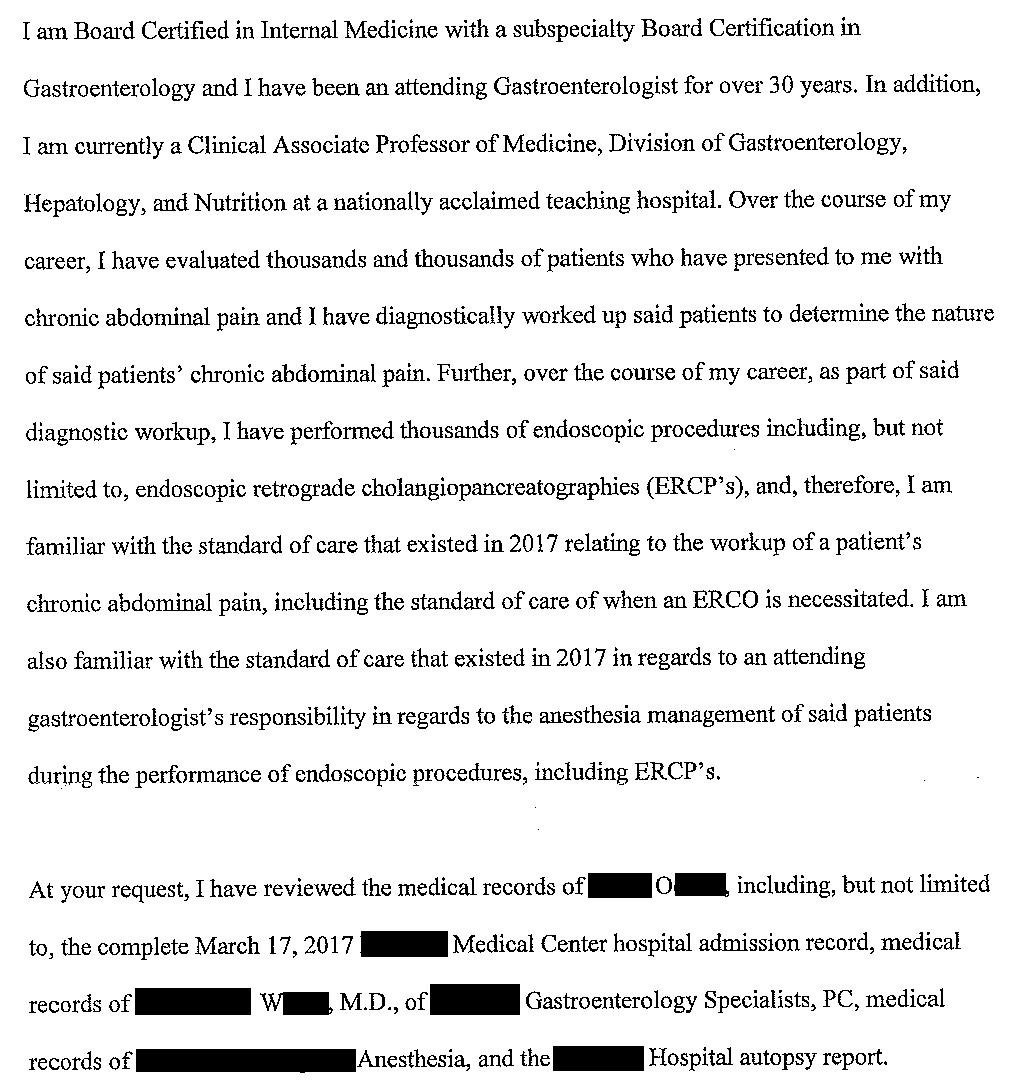
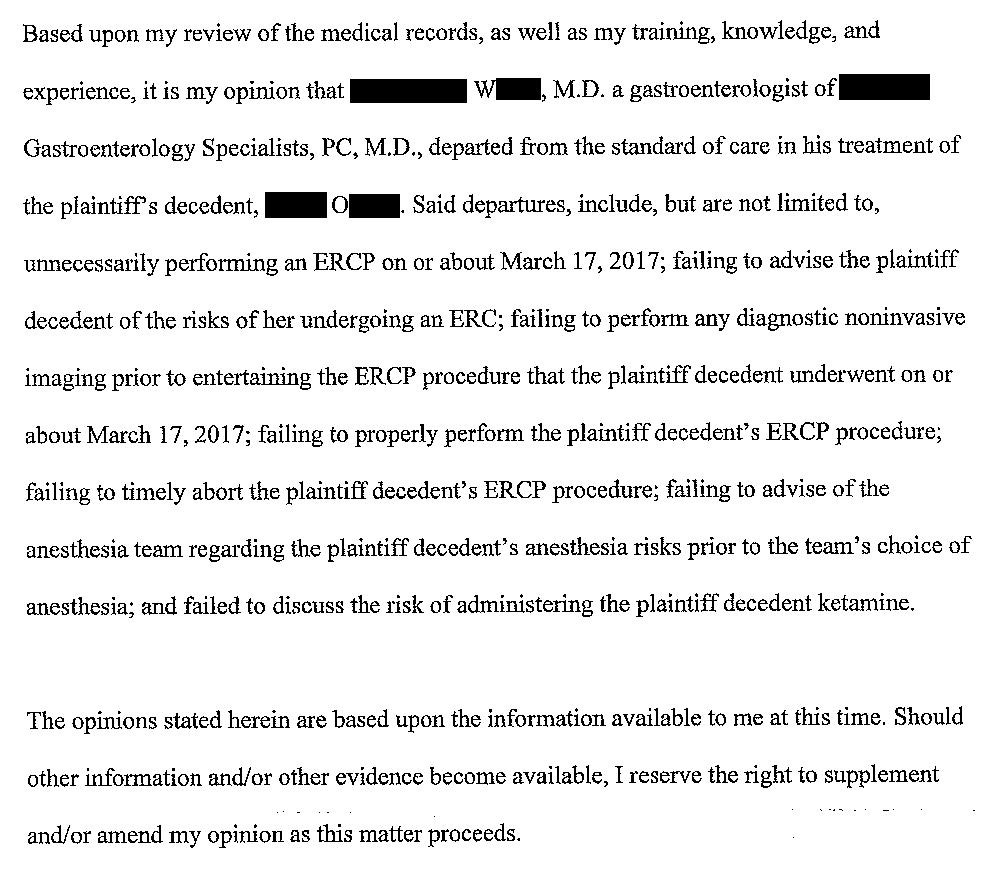
A gastroenterologist wrote the following opinion:
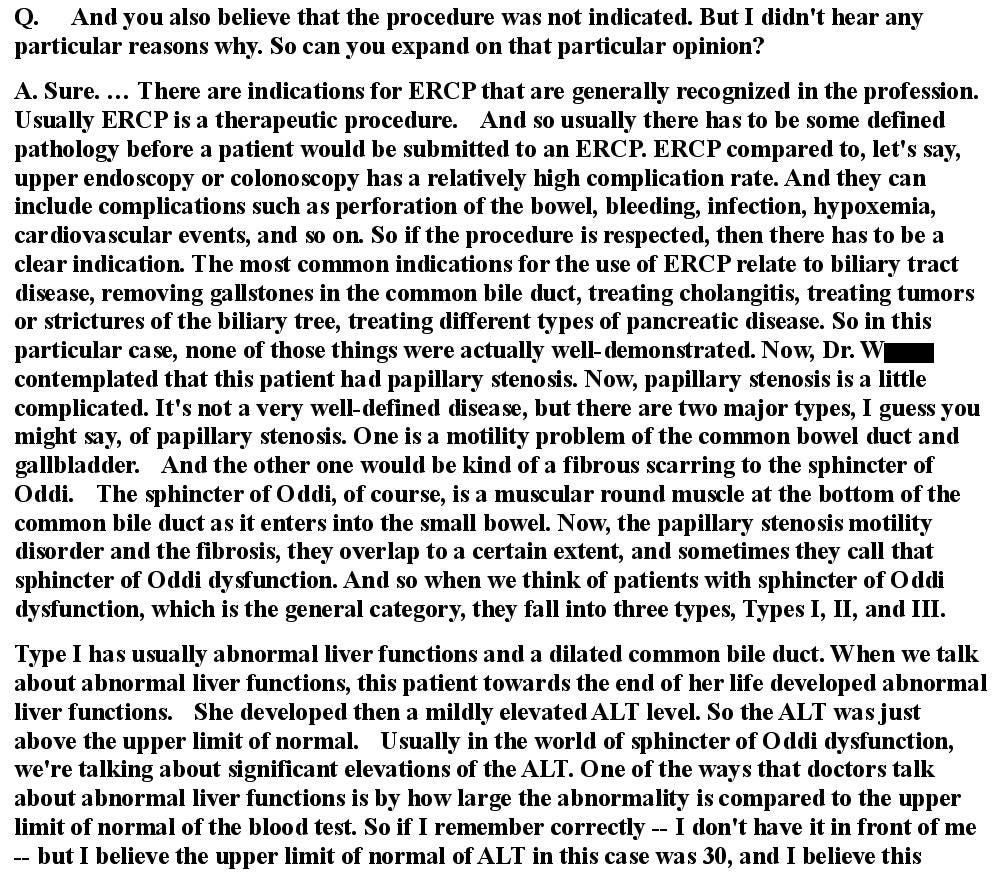
The gastroenterologist elaborated on his opinion during a deposition:
The plaintiffs offered to compromise with the anesthesiologist and his physician group for $1,000,000 each.
They also offered to settle with the GI physician and his group for $1,000,000 each.
The GI physician and his group ultimately agreed to a confidential settlement.
However, the anesthesiologist did not want to settle.
The anesthesiologist’s defense attorney made two strategic moves:
They requested apportionment, which would allow the jury to assign a certain percentage of the liability to the GI doctor. This would allow the anesthesiologist to shift blame to the GI physician, without actually harming the GI physician because he had already settled.
They requested to use the plaintiff’s GI expert. This would functionally mean that the defense would be using the plaintiff’s very own expert against them to prove to the jury that the patient’s death was due to the GI physician’s negligence, not the anesthesiologist.
However, the judge denied both of these requests.
The defendant anesthesiologist (Dr. A) unfortunately passed away in 2021, three years after the lawsuit was filed in 2018.
The lawsuit continued against the Estate of Dr. A and the anesthesiology group.
The case went to a jury trial.
The jury returned a verdict for the plaintiffs, with massive damages.
The defense is appealing on the basis that the judge should have granted apportionment and allowed them to use the plaintiff’s GI expert witness.
Join thousands of doctors on the email list.
MedMalReviewer Analysis:
This is one of the biggest verdicts I’ve seen. It certainly illustrates why sometimes its best to take a settlement offer. They could have taken the plaintiff’s $2,000,000 settlement offer and avoided the stress of a trial, but ended up dragging the lawsuit along for years only to get financially slaughtered by a 8 figure verdict. Its not clear if this will be paid by the anesthesiology group itself, if they have a back-up insurance policy that will pay, or if they’ll end up going after the dead doctor’s estate (which functionally would mean taking money from his widow, a particularly cruel option). Certainly nothing will happen until the appeal is resolved.
The GI doctor was named in another lawsuit that was eerily similar. An ERCP was done, and a patient had a cardiac arrest at the end of the procedure. The anesthesia teams were different between these cases, but it was the exact same GI doctor. Its not clear if this was simply bad luck or if he was practicing in a negligent manner that could have caused both deaths.
The CRNA was being supervised by an anesthesiologist when the hypoxic arrest happened. Unfortunately, the attorneys never specifically described the doses and timing of propofol in this case. The exact level of supervision was also not described in the court documentation. A supervising physician will almost always be named as a defendant in a case involving an NP, PA, CRNAs, or other staff members. In fact, many plaintiffs will not even bother suing the CRNA, and will only go after the supervisor doctor.
One unique thing about this case is the GI expert’s claims that the ERCP should never have been done in the first place. Most malpractice lawsuits related to procedures focus on how the procedure itself was done, not that it was negligent to even attempt the procedure. This case is a poignant example of the hidden risks of ordering more test and doing more procedures. Sometimes the best thing you can do for a patient is nothing at all.






Reason why I intubate most ERCPs
I think criminal charges were reasonable here
Death from Ercp for chronic abdominal pain and normal LFTs is murder in my book.