A 44-year-old dentist (Dr. P) presented to an ENT surgeon (Dr. K) to discuss treatment options for nasal congestion.
Initial treatment attempts with steroid nasal sprays were not successful.
He was diagnosed with a deviated nasal septum, hypertrophic nasal turbinates, and persistent sinusitis.
The patient underwent a surgery by Dr. K, described as “bilateral ethmoidectomy, bilateral antrostomies, endoscopic concha bullosa repair, nasal septoplasty, and internal nasal valve repair”.
The first few post-operative days were uncomplicated.
However, he began having increased sinus pressure.
At some point, the patient manipulated his nose and may have damaged the surgical field.
10 days after the procedure, he developed bleeding that was cauterized with silver nitrate.
Nasal endoscopy revealed a large septal perforation and the middle turbinate was scarred to the lateral wall.
The patient continued to have worsening sinus pressure, headaches, loss of smell, and difficulty breathing through his nose.
Dr. P felt that his post-surgical outcome was far worse than the mildly-annoying sinus symptoms he had been experiencing previously.
He sought second opinions from other ENTs.
They recommended revision procedures to repair the septal perforation.
Protect yourself by reviewing a new malpractice case every week.
Join thousands of doctors on the email list.
Dr. P sued Dr. K, his employer, and the hospital.
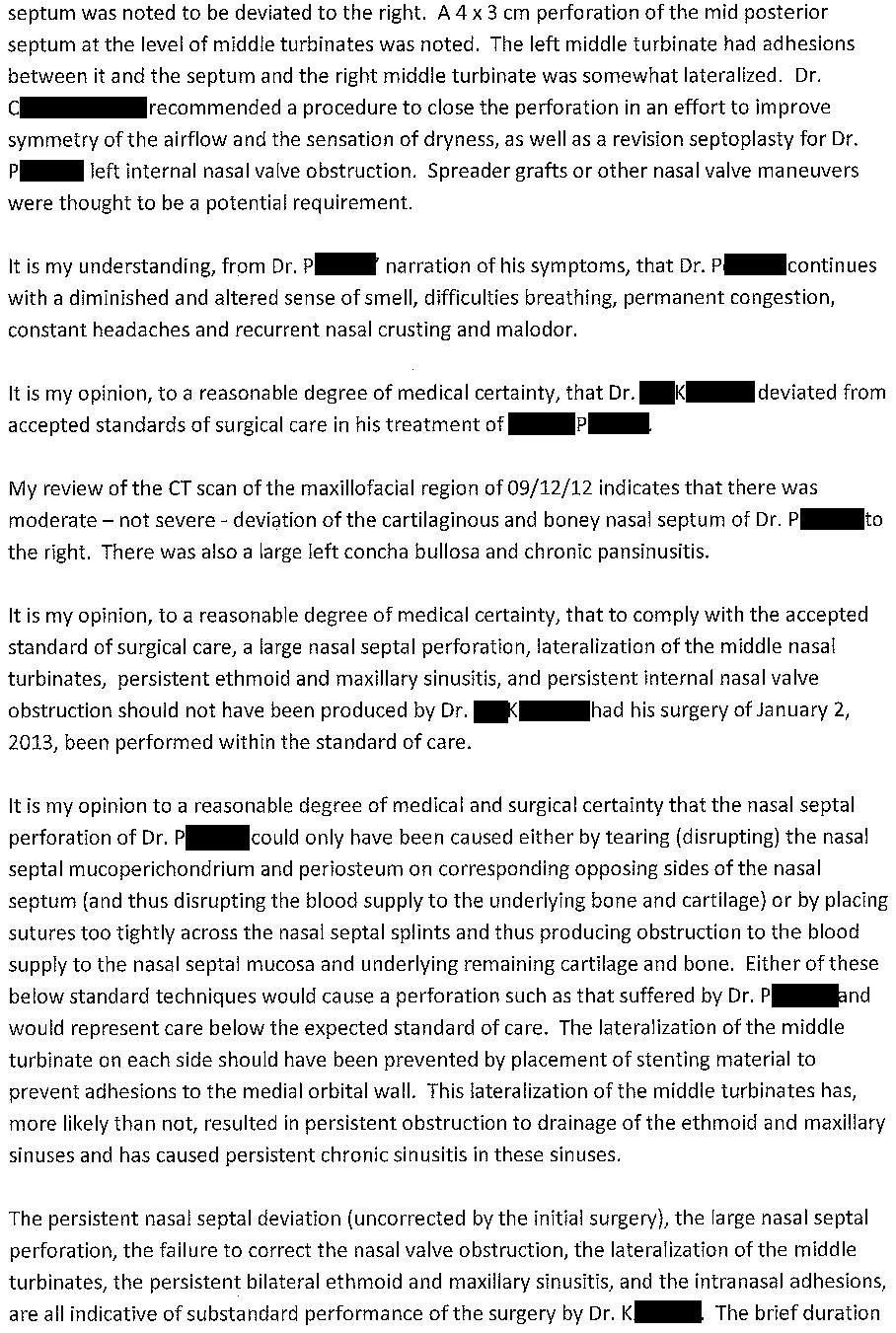
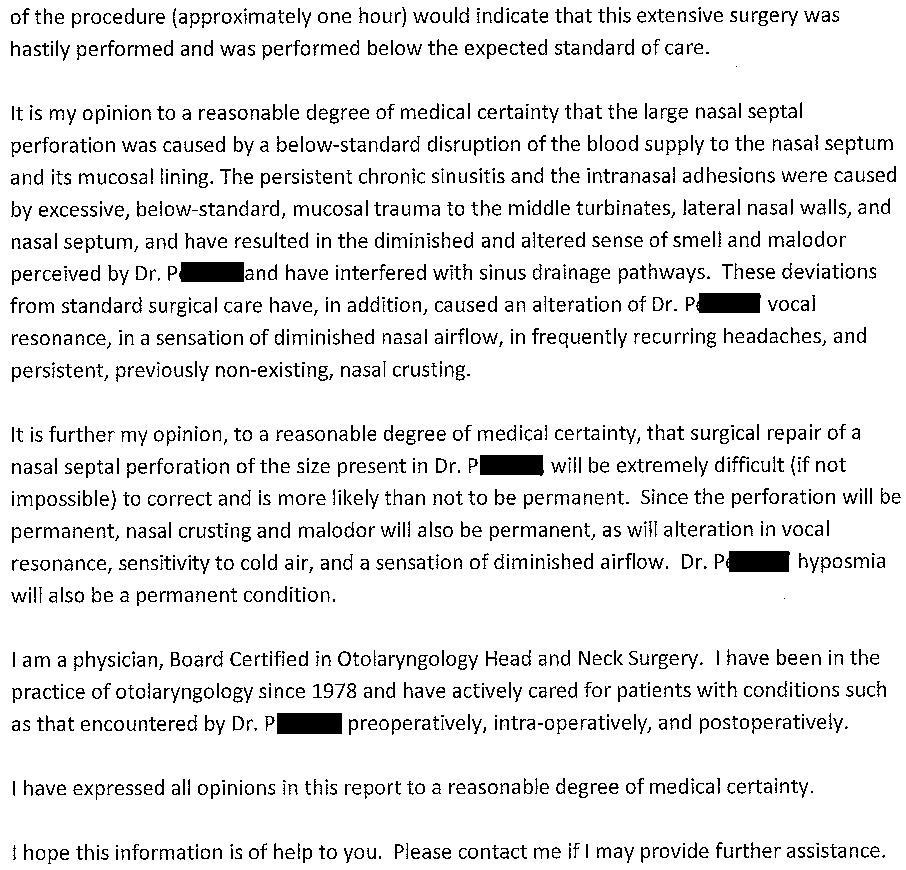
The plaintiff’s ENT expert opinion is shown here:
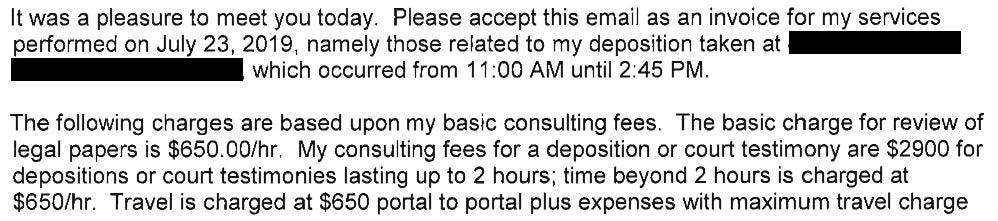
The plaintiff also hired an expert who had a PhD in otolaryngology (Dr. D).
He prepared presentations for the jury about nasal anatomy and was described as “an expert on the sense of human smell”.
He billed the defense attorneys for a deposition that last just under 4 hours.
The defense hired numerous experts, including an ENT physician:
Editor’s Note: Dr. Be is the defense expert and Dr. Bo is the plaintiff’s expert.
Become a better doctor.
Paying subscribers get a new case every week and access to the entire archive.
There is no record of any settlement negotiations.
The hospital and the ENT group were removed from the case.
The case went to trial.
At trial, the testimony of the plaintiff’s non-physician olfactory expert (Dr. D) was severely limited by the judge because he was not an ENT surgeon.
The judge allowed the defense to present evidence that the patient actually caused the poor outcome by manipulating his nose and upper lip, despite requests by the plaintiff’s attorney to ban discussion of this event.
The jury found in favor of Dr. K.
The plaintiff filed a motion asking the judge to set aside the verdict and hold a new trial.
This motion highlights multiple issues that the plaintiffs had with the way the judge presided over the trial.
The judge denied the motion to set aside the verdict and it was finalized.
However, the plaintiffs have now appealed the ruling to a higher court.
Subscribe to get updates when new developments in this case occur.
MedMalReviewer Analysis:
Doctors and other highly educated healthcare professionals can be very challenging patients. They (we) have high expectations and can be more critical of poor outcomes. I would imagine that this patient was consented for risk of perforation, but the patient nonetheless decided to sue. Our peers are often our harshest critics, and this principle applies between colleagues and across the physician-patient relationship. I’ve covered other cases of physicians suing physicians.
The plaintiff claims that his initial symptoms were not severe, and that he simply saw Dr. K to “determine if there was a treatment that could help him”. This phrasing seems to suggest that he was not pushing for surgery, and leads to the implication that it was Dr. K who aggressively pushed him toward surgery. Clear documentation that you discussed the risks with a patient is always important, but especially so when a patient displays any hesitancy. I have a hypothesis that pre-operative hesitancy is strongly associated with increased likelihood of being sued.
I’ve covered malpractice lawsuits related to loss of vision and loss of hearing, but this is the first I’ve covered related to loss of smell. I think we’ll see more and more lawsuits addressing sense of smell (and the appropriate financial compensation if it is lost due to negligence) as tangents to COVID-related lawsuits. The olfactory expert made thousands of dollars on this lawsuit, and is probably well positioned to build an extremely lucrative career as a legal consultant.
The surgery in question happened over 11 years ago and the lawsuit is still active. This is a bit of an anomaly, but it does seem unjust to make both sides wait for decades to reach a conclusion either way.




The technical, visual-spatial and haptic details of this case take years of training to grasp. There is no way that the jury and the judge could have grasped all that with just a few explanations and reports. The demeanor, appearance and speaking style of the plaintiff, experts and lawyers probably determined the outcome of this case.
As physicians I think we expect other physicians to go the extra mile for us. I’ve had good experiences with most of my care. One was bad but I didn’t sue. Luckily the problem was fixed by another orthopedic. Even we can make mistakes choosing the wrong doctor.