A baby girl was delivered by C-section at 26 weeks 6 days gestation for poor fetal heart tracings.
The pregnancy was complicated by severe maternal depression due to a tragic social situation, as well as drug and alcohol use.
The baby had been diagnosed with intrauterine growth restriction.
She weighed 355g at birth.
She was initially on TPN, then transitioned to donor breast milk.
At week 5, formula was introduced.
A few days later, her abdomen was noted to be distended.
She began to have periodic desaturations and bloody stool.
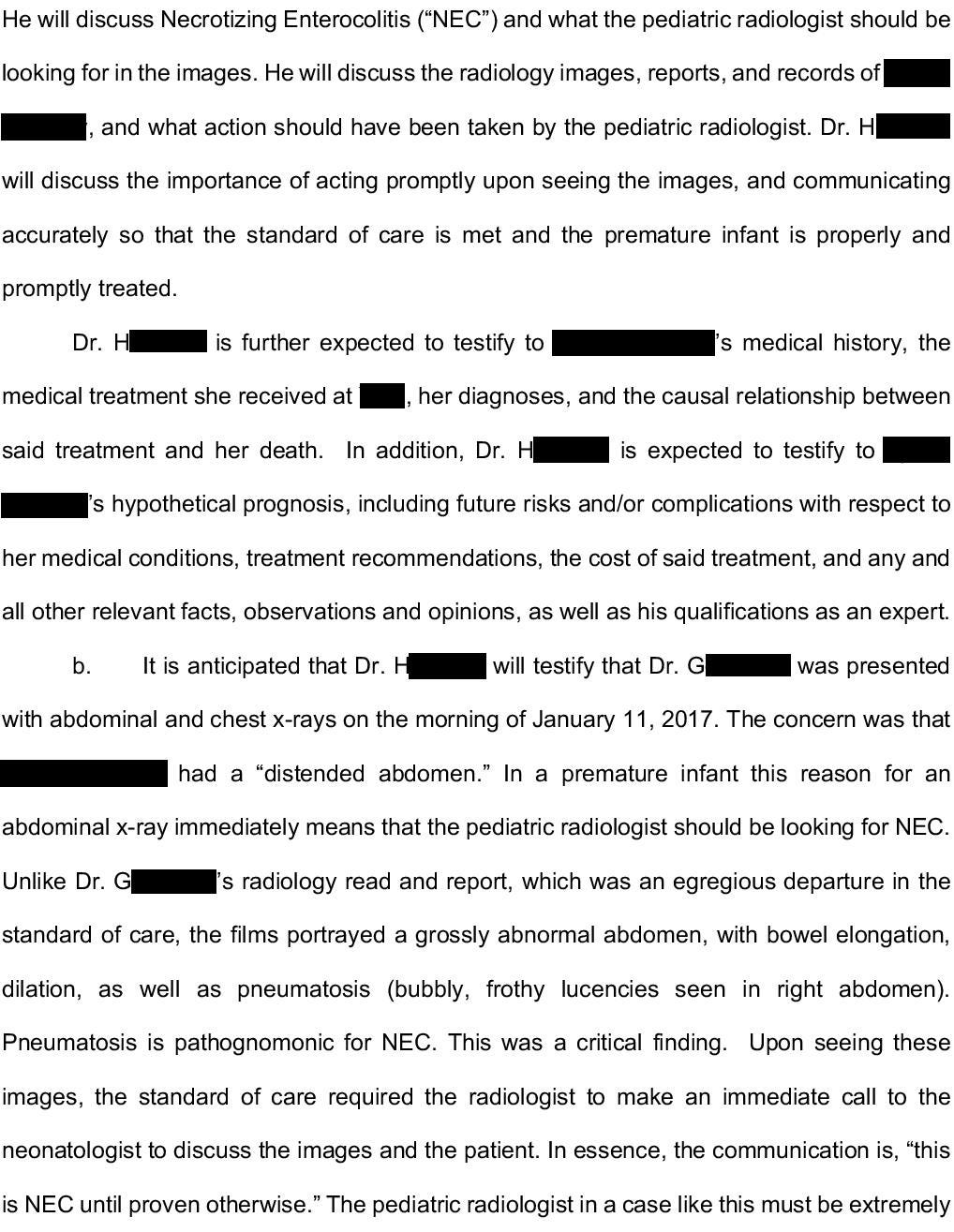
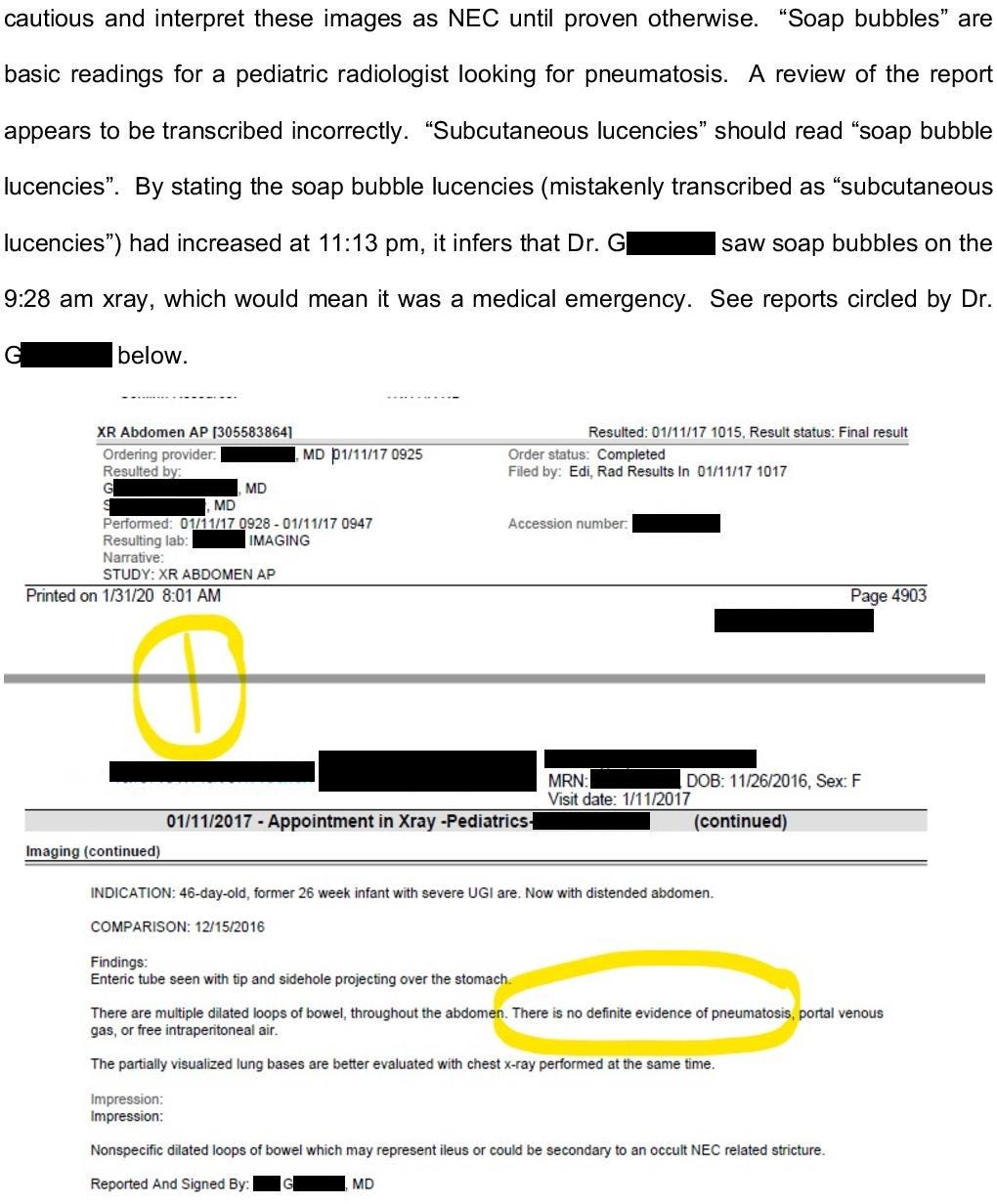
Several x-rays were done, and the radiologist reported nonspecific findings that could be suspicious for necrotizing enterocolitis.
Antibiotics were started and surgery was consulted.
The pediatric surgeon came to the bedside.
An emergency ex-lap was done at the bedside in the NICU.
She was definitively diagnosed with necrotizing enterocolitis.
The patient developed severe acidosis and persistent hypoxia despite full ventilatory support.
Her condition was felt to be futile.
She was transitioned to comfort care and died shortly thereafter.
Join thousands of doctors and attorneys on the email list.
Her mother contacted an attorney and a lawsuit was filed.
Multiple neonatologists were sued, as well as radiologists and the hospital.
The primary criticisms revolved around premature introduction of formula and not identifying NEC earlier on the x-rays.
The defense hired their own neonatologist:
Reviewing lawsuits from multiple different specialties can help us identify trends and themes that affect us all.
Paying subscribers get a new case every week and access to the entire archive.
The plaintiffs hired a pediatric radiologist.
The plaintiff hired an economist, who claimed that the child’s premature death resulted in lost income of $1,148,803.
The defense hired an economist who felt that this was an overestimation of her earning potential.
The plaintiff has offered to compromise for $5,000,000
The lawsuit is ongoing.
Subscribe to be notified of updates as the case progresses.
MedMalReviewer Analysis:
This is the first neonatology case I’ve published. I’ve only seen a few other neonatology cases, but its worth noting that the others I’ve seen have also been about NEC. The other cases I’ve seen all center around the criticism that formula was introduced too quickly and triggered the child’s death.
I didn’t realize that pediatric surgery would do an ex-lap at the bedside in the ICU, but it makes sense given how unstable the patient was. The description of abdominal compartment syndrome with necrotic bowel and multiple perforations paints a poor prognostic picture. I’ve covered 2 previous cases of abdominal compartment syndrome in adults (here and here).
The lawsuit was initially filed in 2019. All of the doctors were voluntarily dropped from the case within the first few weeks. It appears that the plaintiff’s attorney planned to go after the hospital all along, given that they have a bigger insurance policy than any individual doctor.










We pediatric surgeons operate at the bedside not infrequently for several reasons. First, many are too unstable to transport, as was pointed out. Second, the child often gets very cold in transport and in the large OR. The NICU has radiant warmers built into most of the beds to mitigate this. Third, it's not uncommon for the child to be on an oscillator or jet vent and there often isn't time to "trial" the child back on a conventional vent, as would be needed for the anesthetic carts in the operating room. And so we bring the OR to the patient...
It is difficult to predict who will get "medical NEC" and need only bowel rest/antibiotics to recover and who will develop a rapid, fulminant NEC requiring surgery or leading to death. Peds surgeons often state its about 1/3 medical, 1/3 surgical, and 1/3 fatal. Early KUB's of NEC can be difficult in that pneumatosis and the "bubbly" look of neonatal poop are sometimes challenging. It gets more obvious with sequential imaging. While most of us repeat films every 6-8 hours on a patient with possible pneumatosis, that's based on common practice, not data. Additionally, surgery doesn't stop or "fix" NEC. We operate for the complications of NEC - full thickness perforation (or suspicion of it), severe deterioration despite optimal medical management (two pressors, acidosis, 100% fio2 and getting harder to ventilate), and abdominal compartment syndrome (as in this patient). It might have been good to call surgery to see them a little earlier. However, with portal venous gas on the first convincing film, the prognosis was already poor in this uber premature kiddo. I don't have an issue with use of fortifiers. I have a personal bias against 30 kcal formula in a micro-preemie (I max out at 27 kcal), but you can find data both for an against that.
If I was sitting on the panel, I'd offer $1 million to make the case go away. $5 million is a bit high for no clear error in care. Just my two cents, and I'm pretty new at the expert witness field.
It is hard to judge without seeing the kub being referenced as early signs of NEC. It is plausible to also question why they waited 12 hrs for a repeat x-ray. that being said this baby was most likely not going to make it even if they had diagnosed him 6-12 hours prior. It seems absurd to put all blame on the medical team for this baby's misfortunes when it's clear the baby wouldn't have made it a day without all their hard work and extreme interventions. Mom trying to get rich from this after self sabotaging her own pregnancy is quite disturbing. I wonder how much lawyers are allowed to say regarding this.