I published this case about intrahepatic cholestasis of pregnancy back in April 2022.
A 27-year-old woman had developed pruritis at 32 weeks gestation.
She was initially started on ursodiol 300mg BID, but bile acid levels came back normal.
After several more visits, her pruritis was noted to be worsening at 35 weeks.
Her OBGYN told her to re-start ursodiol and sent repeat labs again.
The patient allegedly did not re-start ursodiol as instructed.
The bile acids were a send out lab that took a week to come back.
She presented to L&D several days after the lab draw, and was diagnosed with fetal demise.
The bile acids came back critically elevated at 137.7 several days after fetal demise.
When I originally published the case, it was still pending.
Both OBGYNs who saw her were removed from the case (I suspect they settled but there was no official confirmation in court records).
This left their medical group and the hospital as the sole defendants.
Become a better doctor by reviewing malpractice cases.
Paying subscribers get a new case each week and access to the entire archive.
The lawsuit went to a jury trial.
Part of the defense strategy was to argue contributory negligence on the part of the patient.
They pointed out that she did not show up for her glucose tolerance test appointments, and did not take ursodiol as prescribed.
However, part way through the trial they withdrew their claim of contributory negligence.
After 3 weeks, a mistrial was declared (for reasons not described in court documents).
After the mistrial, Dr. B and the patient had a short conversation. Neither attorney overheard the nature of their discussion.
A new trial was started.
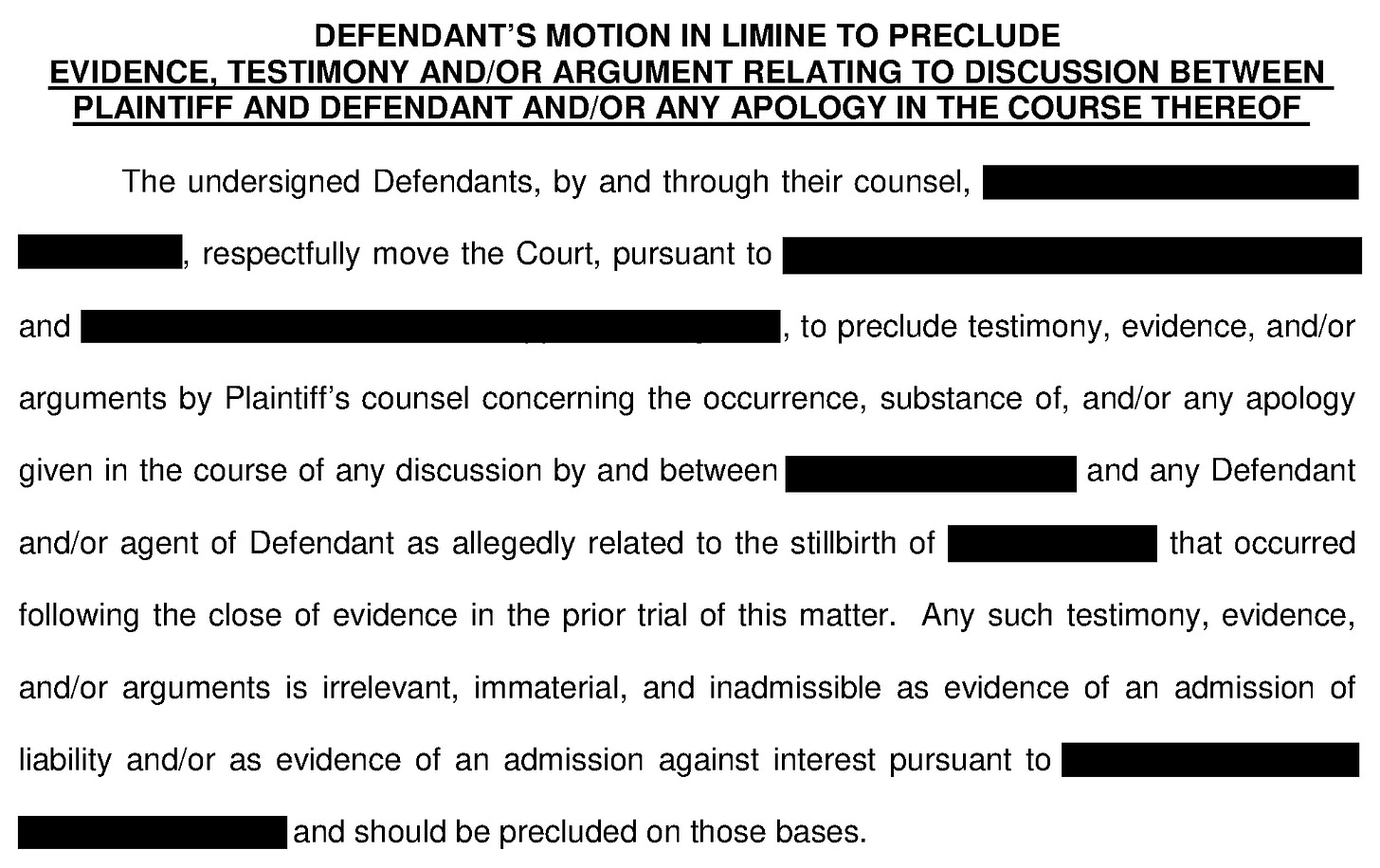
The defense was worried that Dr. B had apologized to the patient after the mistrial, and requested that the judge ban any mention of this theoretical apology.
The judge ruled that the plaintiff would need to disclose any proof they had of an apology prior to the next trial, and that he would make a decision at that point.
The plaintiff never offered any proof of an apology and it was not mentioned at the second trial.
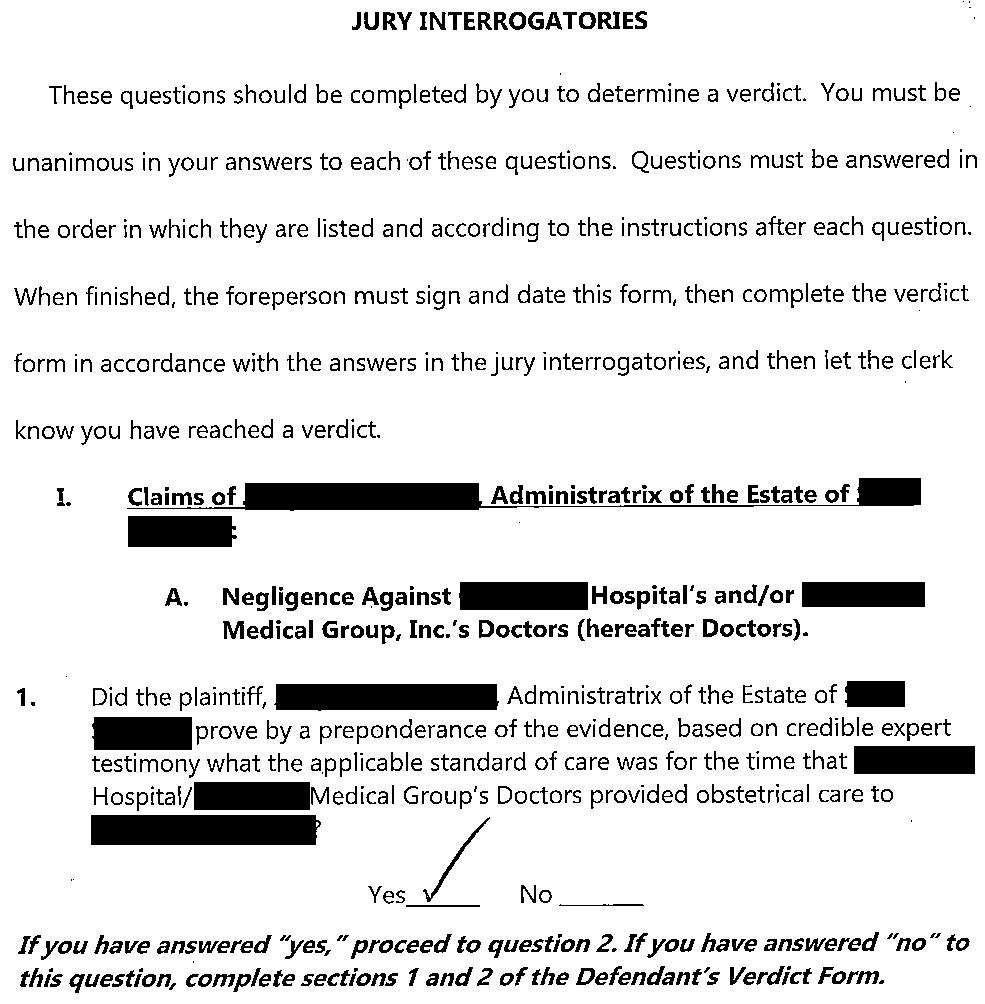
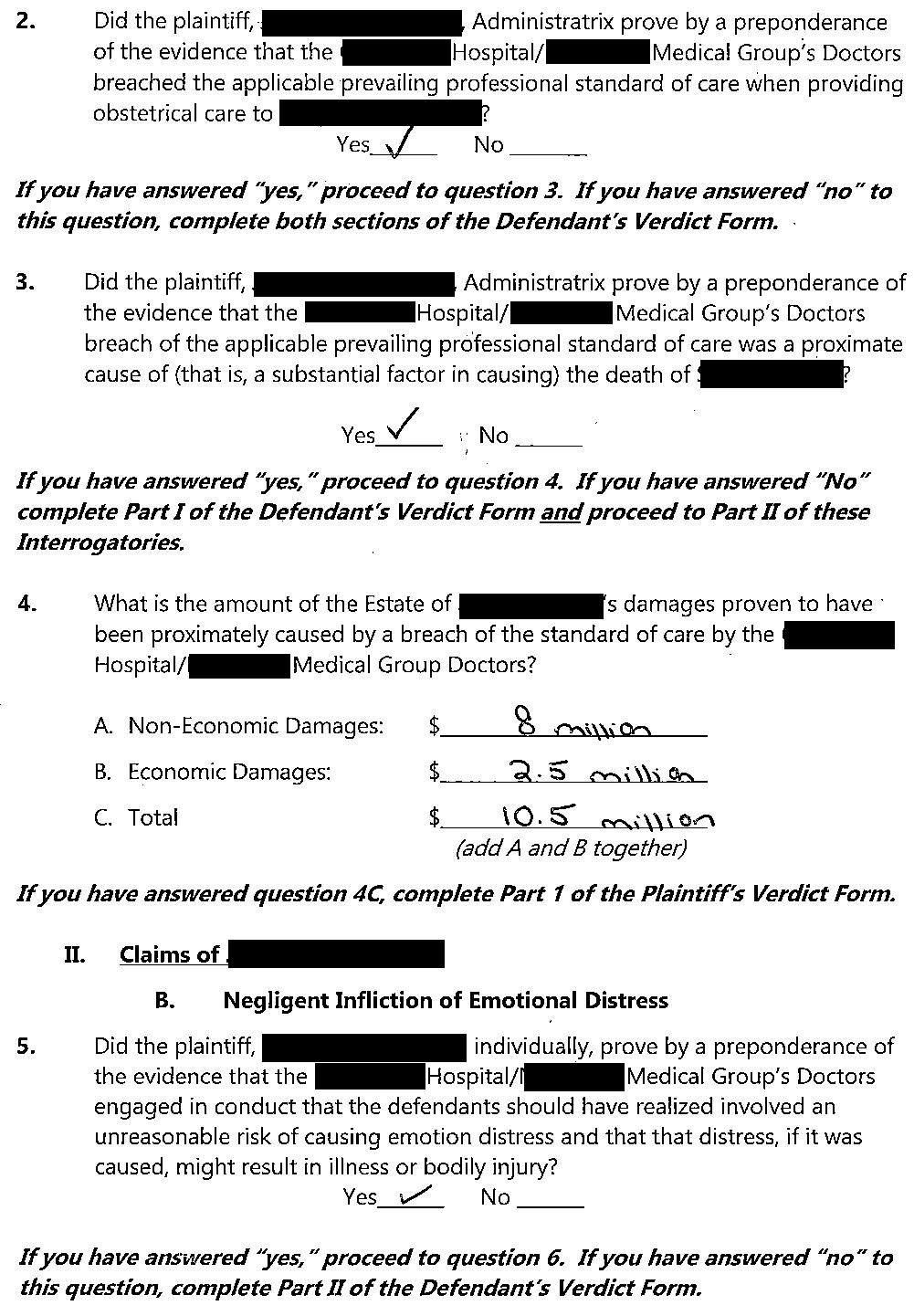
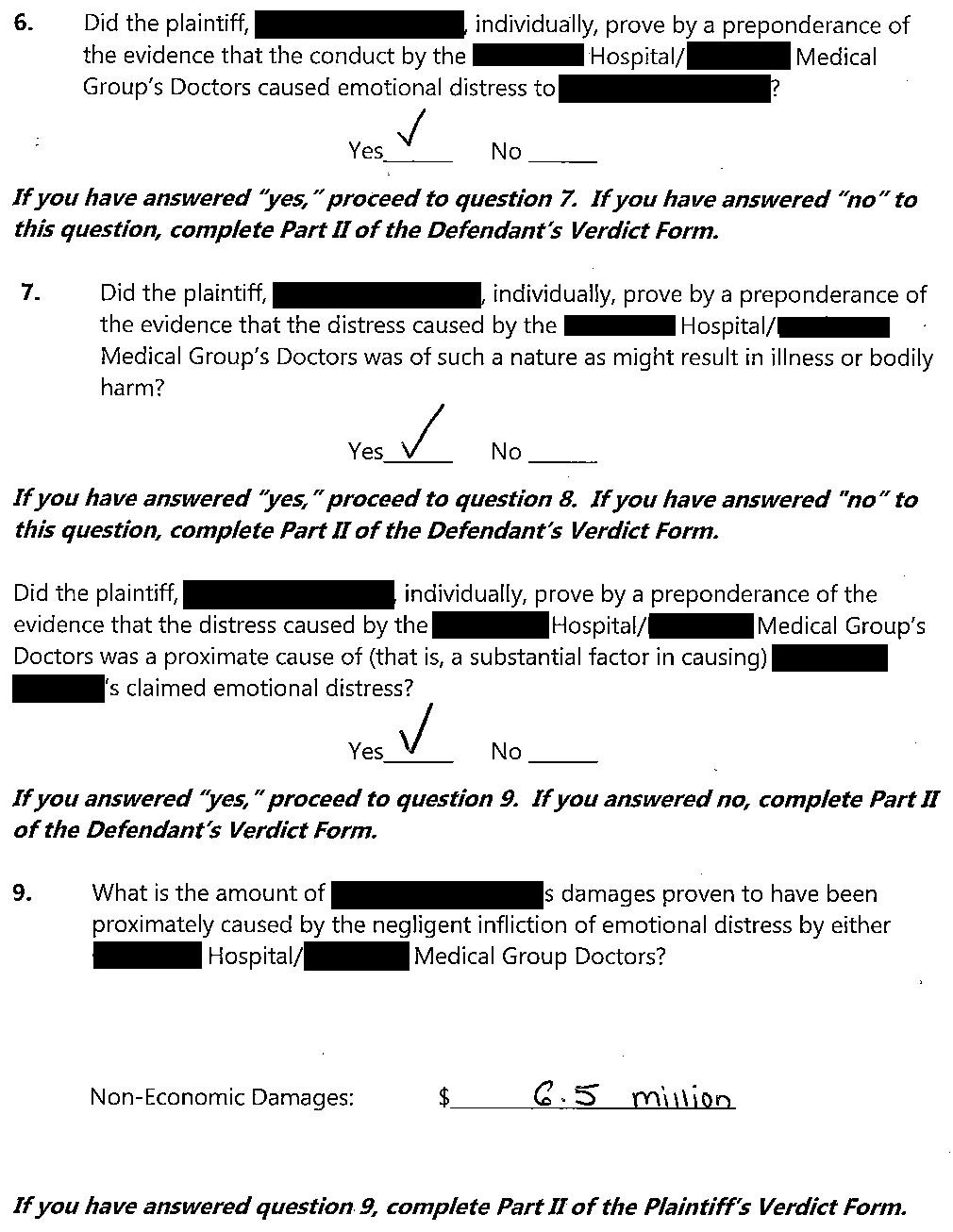
At the second trial, the jury returned a verdict in favor of the plaintiff.
They awarded $10,500,000 to the estate of the deceased baby and $6,500,000 to the mother.
The verdict was appealed.
Both sides reached a settlement prior to completion of the appeals process.
Protect yourself by reviewing new lawsuits every week.
The unique thing about learning from malpractice cases is that the learning pearls apply broadly to doctors of all specialties, even when they’re outside your area.
MedMalReviewer Analysis:
If you read my analysis back on the original case in 2022, I guessed that the case would settle before trial. My guess was wrong! I think the hospital probably wishes they had settled earlier, although admittedly there are a lot of variables that we just don’t know that could have affected this decision:
How much was the pre-trial settlement offer?
How much were the offers between the two trials?
How much did they actually settle for during the appeal of the $17,000,000 verdict?
This what the plaintiffs are really aiming for - finding the hospital liable for a massive verdict, not the individual doctor. The hospital is the defendant with the biggest insurance policies and deepest pockets, far bigger than any individual doctor. They’re primarily coming after your hospital and/or your insurance policy, you are only a pawn in their game. Keep that in mind. A few weeks ago I posted an update about the ER doctor who was found liable for 60% of a $75,000,000 verdict, and yet the plaintiff appealed because the hospital was let off the hook… it’s the exact same principle here. They know they can get the money from the hospital, but probably can’t from a doctor. When you get sued (we pretty much all will), keep this in mind when you’re asked if you want to settle or not.
I’m curious about the defense strategy to advance a theory of contributory negligence throughout the entire multi-year pre-trial period, through most of a trial, then suddenly drop it. Patients who cause their own bad outcome by ignoring a doctor’s advice shouldn’t be able to blame doctors when something bad happens… But on the flip side, trying to blame a patient if they actually got bad care from their doctor is unethical. Not to mention the fact that a doctor who is trying to blame a patient for their own shortcomings is likely to inflame the passions of a jury and make them incredibly mad at the doctor.




As someone in OB... intrahepatic cholestasis of pregnancy has known risk of stillbirth. Ursodiol improves symptoms and lab abnormalities but doesn't seem to decrease risk for stillbirth. We do antenatal fetal surveillance in these patients, but stillbirth in ICP is probably a sudden event rather than a chronic process and there may not be preceding signs on a weekly ultrasound. The bile acids are always send-out.
Maybe she should have been delivered earlier based on the LFTs, like the expert opinion suggests. But patients who refuse recommended interventions in pregnancy really tend to refuse preterm delivery.
Anyway, no one wants to accept that there are rare, terrible things that can happen in pregnancy that we cannot perfectly prevent.
I still haven't fully digested this case. My ex and I lost our 1st baby (blighted ovum) very early in pregnancy so admittedly my situation is vastly different than losing a near term pregnancy of what appears to have been a perfectly viable baby. It was easy for me to brush of my loss, saying, "hey that's nature and proceeded with a D&C in the OB office. Pregnancy and childbirth have never been without risks and that was oh-so-true back a hundred years ago when a certain percentage of mothers died during or after childbirth, and of course, the baby too in some cases.
But the pendulum has swung the other way. Here this mother has had oodles of ED and OB visits, labs, ultrasound etc. The system has become so complex that it has become a damned if you do, damned if you don't situation in which only the parasitic lawyers win, taking at a minimum 33% of the "loot." They don't give a damn about their clients. They use them only as means to make money off the system.
I could see if this was an outrageous case of gross medical malpractice like decapitating a baby with a botched forceps delivery instead of the C section. (There was a case like this.) There were some factors which complicated this, like depending on outsourced labs, non compliance with urodiol.
In my memoirs I summed up my disgust: It is the paradox of progress: Never has the medical field been able to do so much for so many people, yet never have people been so ungrateful. "We want the latest and most expensive technology. We don't care how much it costs and we shouldn't have to pay for it. And we want it NOW, without having to wait. And if the hospital or doctor makes even an honest mistake, we want to be able to sue them for everything they've got. The fact that we are overweight, smoke, drink, and get no exercise is no excuse. "
Nothing is mentioned about this patient's own dietary, exercise or social Hx, etc. For starters, what was her pre pregnancy BMI? Cholestasis? As I recall from medical school , the mnemonic was FAT, female forty and fertile. How fat? She isn't even thirty.
As an admittedly disgruntled orthopedic surgeon whose career was ruined by an RN's premeditated mistake ( delegating behind my back a tech to select and draw up a drug I for which I had given a direct verbal order to the RN in the OR which she acknowledged, had written on her scrubs and read back to me verbatim, turned out to be a lethal drug retrieved by the tech. The tech testified she "didn't know what drug she was supposed to get." The RN didn't check and knew immediately she had violated her most sacred trust. Her testimony " There goes my license." I got my license suspended by the KY Medical Board.
NOTHING happening to the nurse or tech. I have very little empathy or sympathy for the public. They need to see what it's like when they have no health care. I've seen it in rural India, Philippines and Africa.