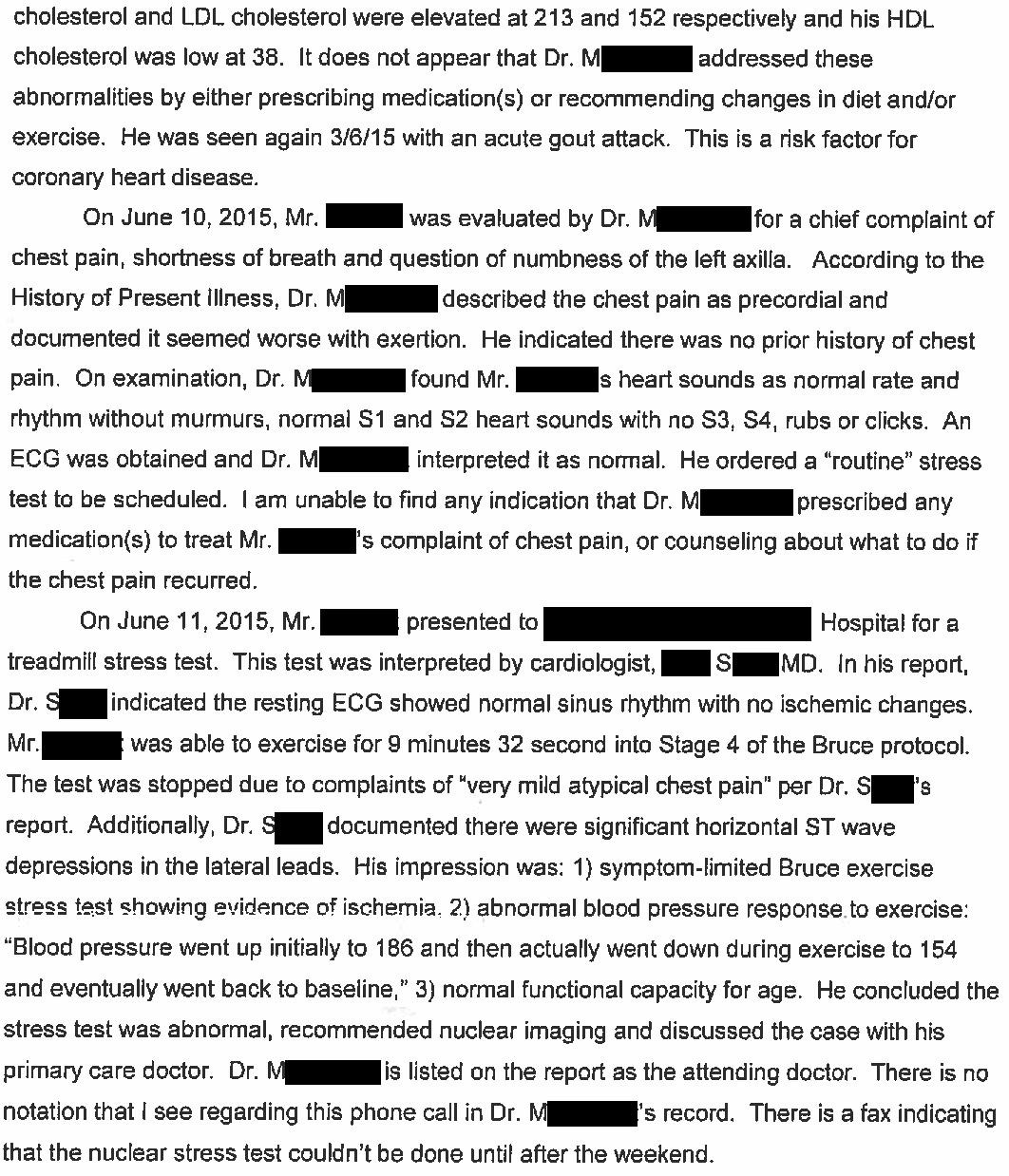
A 58-year-old man presented to his primary care physician (Dr. M, trained in Family Medicine) with several days of chest pain and shortness of breath.
These symptoms occurred with exertion.
He had not been worked up for coronary artery disease previously, but did have risk factors.
An EKG was reportedly unremarkable.
Dr. M ordered a stress test.
A treadmill stress test was completed the next day.
The cardiologist (Dr. S) noted ST elevations in aVR and depressions in the lateral leads.
The patient developed “very mild atypical chest pain”.
Dr. S discussed the results with Dr. M.
He recommended a nuclear stress test, which was scheduled for the following week.
2 days later, the patient had a sudden cardiac arrest at home.
He was briefly resuscitated but ultimately died.
An autopsy was done which showed 3-vessel disease:
85% occlusion of the LAD
50% occlusion of the left circumflex artery
80% occlusion of the right coronary artery
Join thousands of physicians and attorneys on the email list.
A lawsuit was filed against Dr. M (PCP), Dr. S (cardiologist), and the hospital that employed them.
The plaintiff hired a Family Medicine physician:
The plaintiff’s law firm also hired a cardiologist:
Want to review more malpractice lawsuits?
Paying subscribers get a new case every week and access to the entire archive of previous cases.
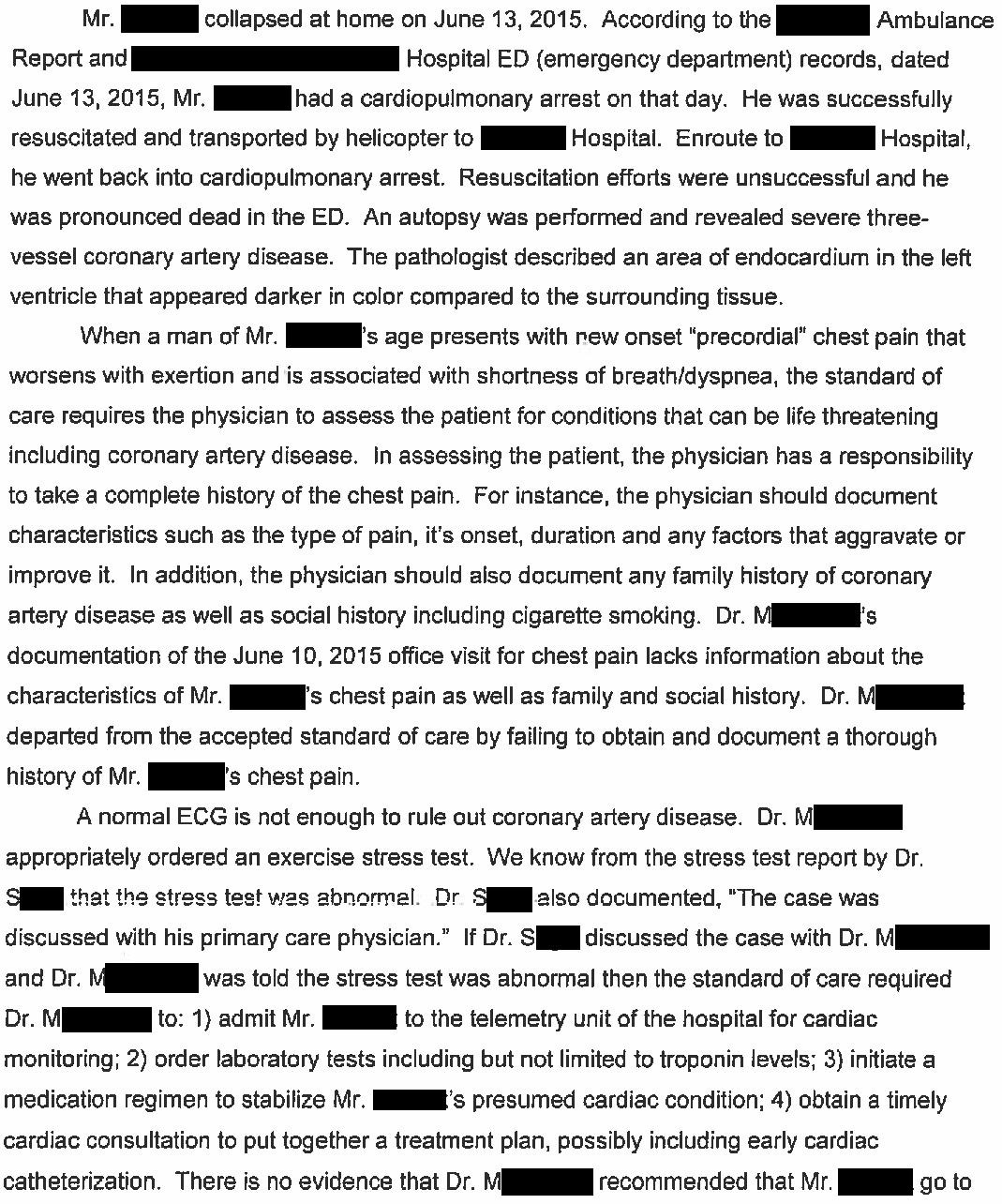
The defense hired multiple experts to defend Dr. M and Dr. S.
A summary of their cardiologist’s opinion is shown here:
They also hired several primary care experts, but their reports were not filed into the public court records.
6 years after the lawsuit was filed, a confidential settlement was reached.
MedMalReviewer Analysis:
The plaintiff’s cardiologist noted that the EKG pattern described during the stress test (ST elevation in aVR and depression in multiple other leads) is classic for left main, proximal LAD, or severe triple vessel disease. This LITFL article has an excellent overview of the topic. I have no doubt that the defending cardiologist was familiar with this pattern.
One of the key issues in this case is what to do with patients who have an abnormal stress test but no chest pain at rest. The plaintiff’s expert suggests that these patients should immediately be admitted for an expedited catheterization. It seems that this would place significant additional strain on the (already overburdened) ED and hospital. In my experience, most of these patients have a scheduled catheterization.
The criticisms of the primary care physician seem overly aggressive. Taking a good history is important, but the fact that Dr. M didn’t document the exact details of his pain did not cause the patient’s death. The expert also stated that Dr. M should have immediately admitted the patient and consulted a cardiologist. This seems like a foolish accusation given that Dr. M spoke with the cardiologist about the case and there was a clear recommendation and plan.
The patient was noted as having chest pain prior to the cardiac arrest. He should have returned to the ED immediately if he was having worsening or escalating chest pain (especially in light of the abnormal stress test). It’s unclear if the patient was given appropriate counseling about this, or if he simply ignored the chest pain for some reason. The defense did not raise the issue of contributory negligence.
I’ve covered a previous lawsuit regarding a positive stress test with allegedly inappropriate follow-up:
Unfortunately, lawsuits related to stress tests are relatively common. I have 3 more that I’m monitoring and will publish once they reach a conclusion.
Join the email list to be notified when they’re published!




Two points:
1. It’s unclear to me that the cause of death was CAD. The greatest degree of stenosis was 85%, if the cause of death was CAD shouldn't there be a 100% occlusion?
2. On the other hand, I do think that the patient should have been admitted after the abnormal stress test. As an ER doc I’m relatively liberal with discharging patients with chest pain, but I absolutely would have admitted this patient, and I’m curious what the troponin levels would have been. Although it’s not typically done, maybe outpatient troponin levels in this case would’ve been better than not doing them at all.
2 of the very first things I learned about the heart were 1) new onset chest pain in a middle aged man is coronary disease till proven otherwise; and 2) the "R" in avR stands for "RESPECT." I think a good case can be made for going directly to cath with that ETT. Yes, hospitals are overburdened, but people get admitted for far less worrisome reasons.