A 27-year-old woman at 7 weeks 0 days by LMP presented to the ED with abdominal pain.
She had taken an at-home pregnancy test that was positive.
She had not yet established with an OB.
The ultrasound showed a single intrauterine pregnancy.
She was discharged and referred to OB.
The following weeks were relatively uneventful.
She was seen by her OB at multiple visits and had an ED visit for vaginal bleeding but no serious complications were discovered.
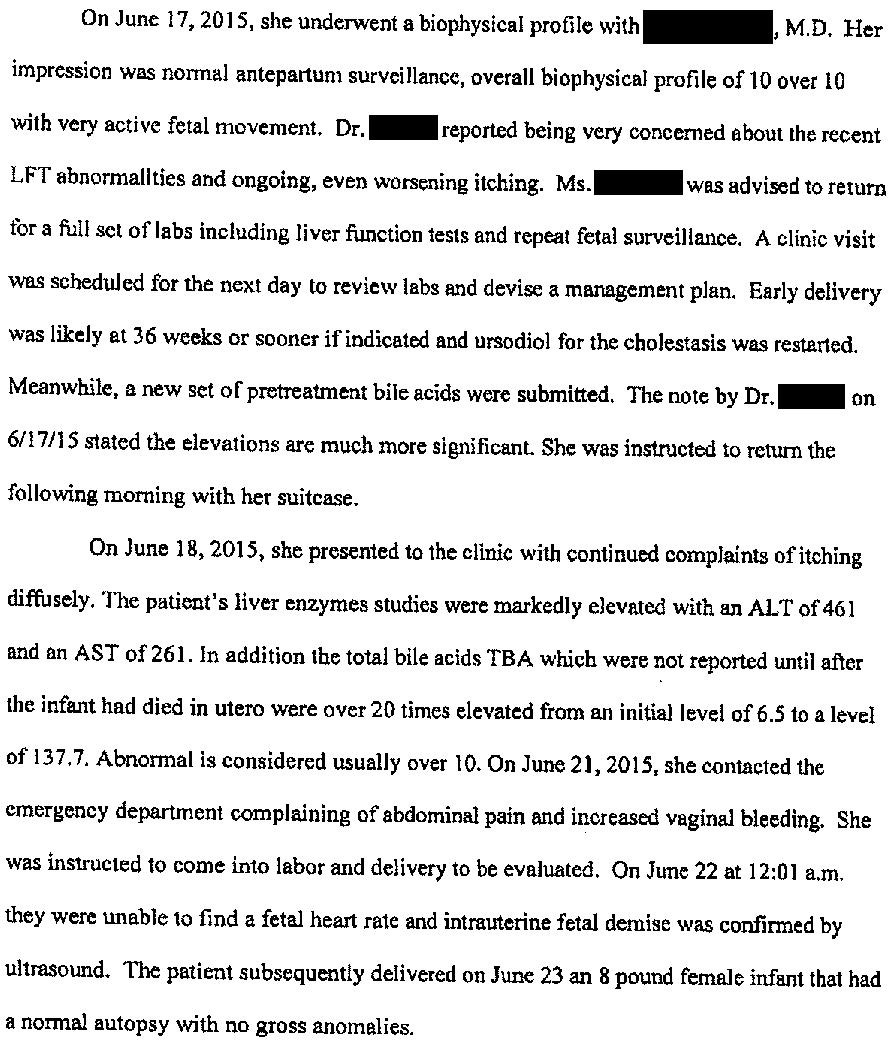
At 32 weeks she developed diffuse pruritus.
She was presumptively diagnosed with intrahepatic cholestasis of pregnancy.
Ursodiol 300mg BID was started.
Labs were ordered.
When they came back the next day, the bile acid levels were normal.
Therefore, she was told that she did not actually have ICP and to stop taking ursodiol.
The patient continued to report pruritus.
Her OB re-started ursodiol several weeks later after becoming concerned that she did in fact have ICP.
She ultimately presented back to the ED at ~35 weeks with abdominal pain and vaginal bleeding.
She was sent to L&D.
Tragically, there was no fetal heartbeat and she was diagnosed with fetal demise.
The patient was understandably shocked and upset.
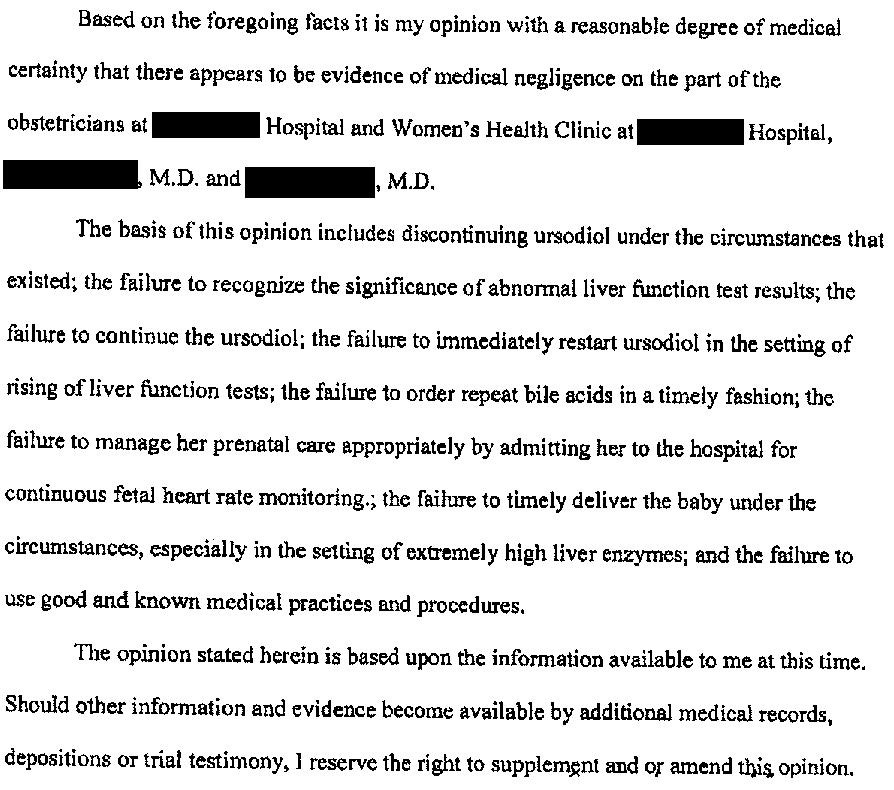
She contacted a law firm and a lawsuit was filed.
They sued both OBGYNs she saw (Dr. A and Dr. B), their medical group, and the hospital.
The expert witness opinion is shown here.
Both OBGYNs settled before trial.
This left their medical group and the hospital as the sole defendants.
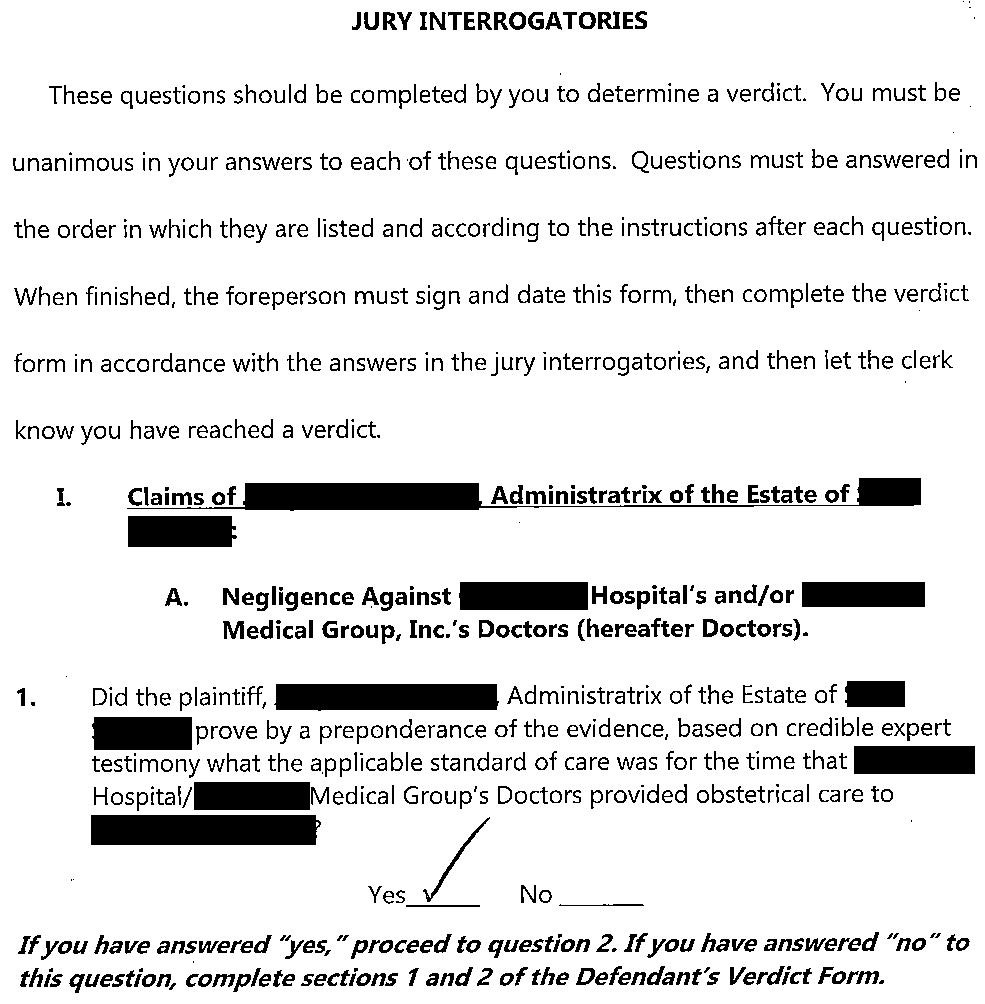
The lawsuit went to a jury trial.
Part of the defense strategy was to argue contributory negligence on the part of the patient.
They pointed out that she did not show up for her glucose tolerance test appointments, and did not take ursodiol as prescribed.
However, part way through the trial they withdrew their claim of contributory negligence.
After 3 weeks, a mistrial was declared (for reasons not described in court documents).
After the mistrial, Dr. B and the patient had a short conversation. Neither attorney overheard the nature of their discussion.
A new trial was started.
The defense was worried that Dr. B had apologized to the patient after the mistrial, and requested that the judge ban any mention of this theoretical apology.
The judge ruled that the plaintiff would need to disclose any proof they had of an apology prior to trial, and that he would make a decision at that point.
The plaintiff never offered any proof of an apology and it was not mentioned at the second trial.
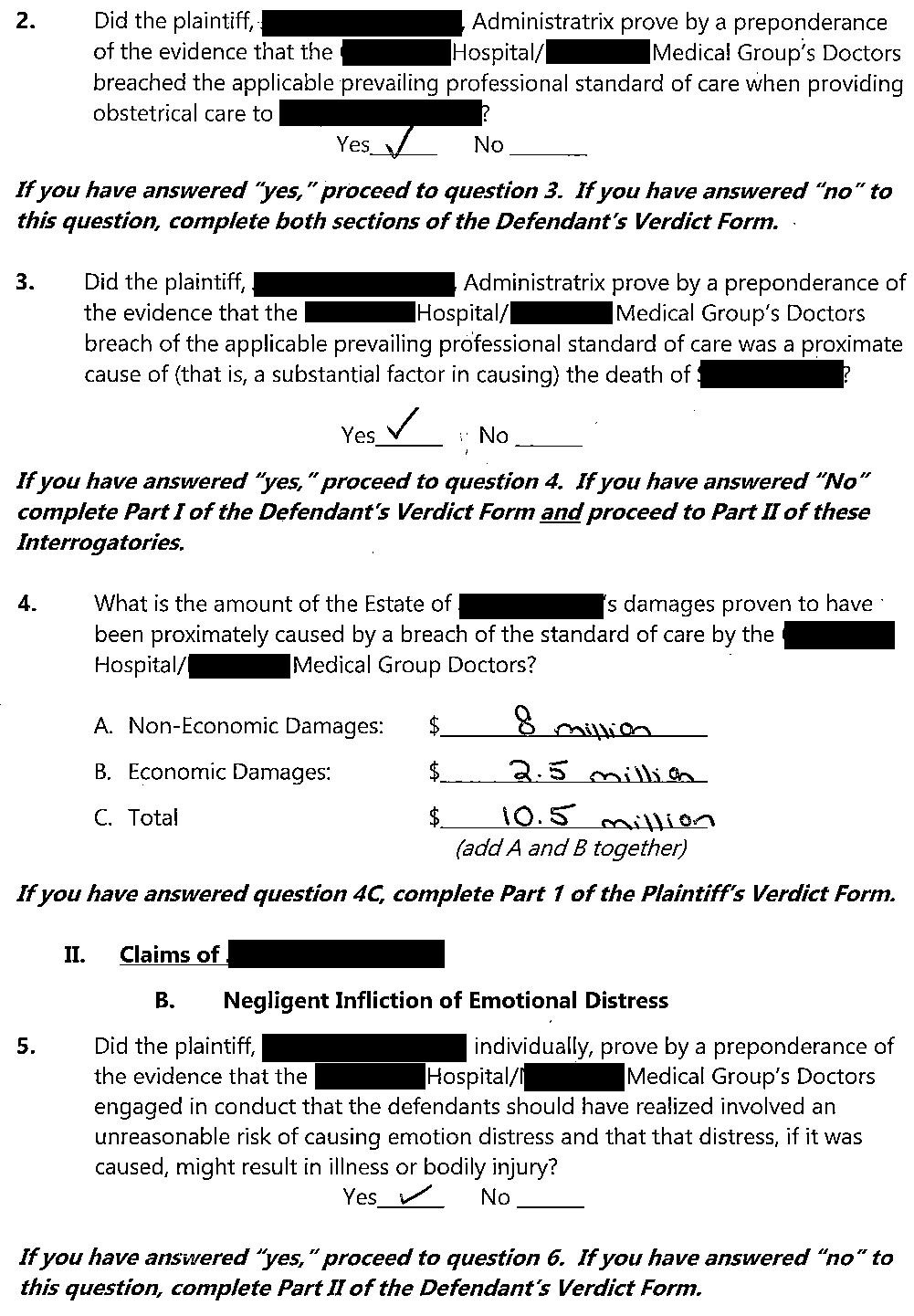
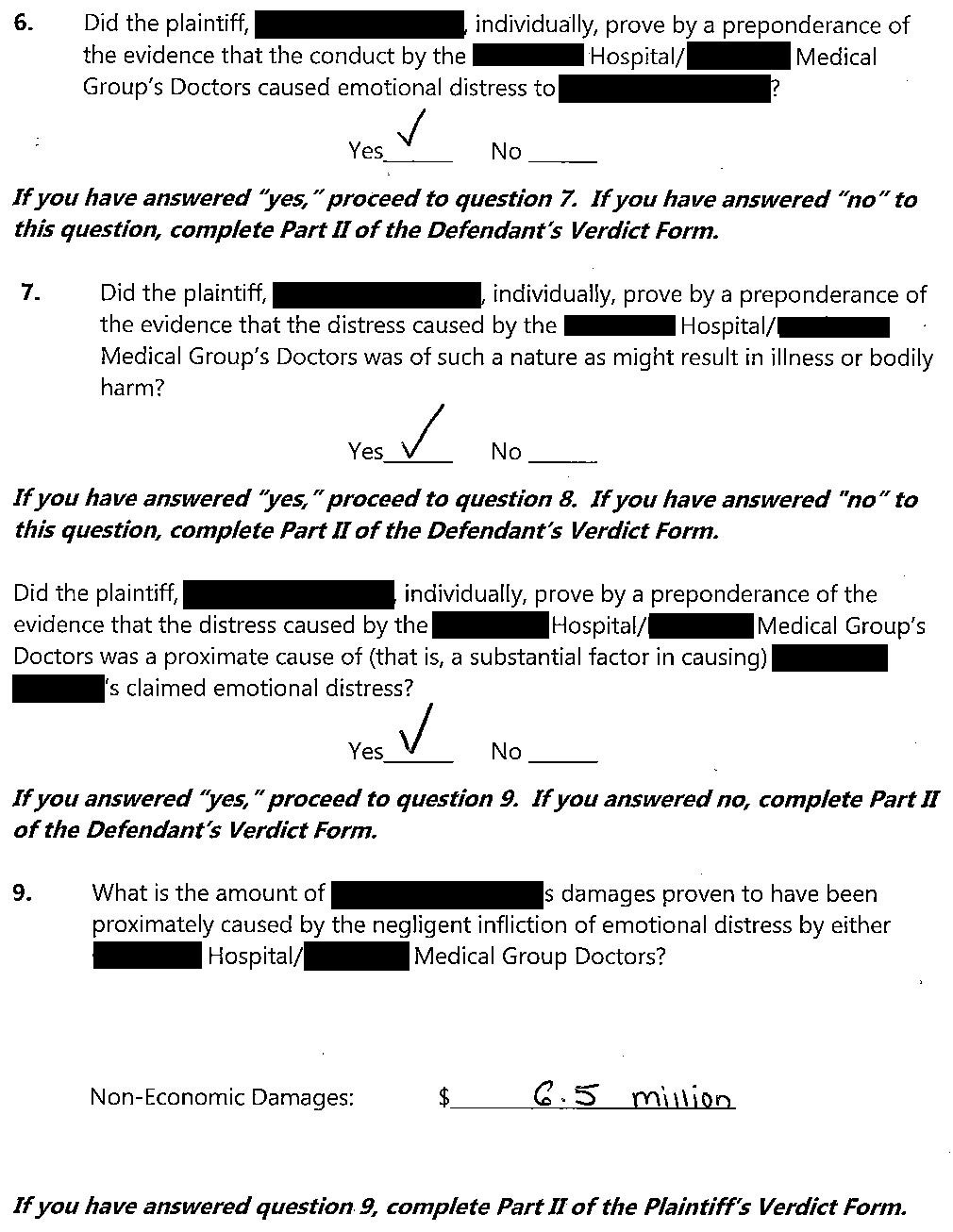
At the second trial, the jury returned a verdict in favor of the plaintiff.
They awarded $10,500,000 to the estate of the deceased baby and $6,500,000 to the mother.
The verdict was appealed.
Both sides reached a settlement prior to completion of the appeals process.
Upgrade to a paid subscription to get updates on cases, access to the entire archive, and to expand your medicolegal expertise through consistent weekly case review.
MedMalReviewer Analysis:
OB lawsuits are common but often not applicable to a broad audience. I have more OB lawsuits than any other specialty.
This case is unique because the patient had multiple points of contact with non-OB physicians (ED and primary care visits). Intrahepatic cholestasis of pregnancy is an uncommon entity and important to keep in mind for generalists.
This is an excellent (and short) review article for those who want to read more.
In some ways, the financial risk to the defendant is slightly lower in this case than other OB lawsuits because there is not an injured plaintiff that will require a lifetime of care. However, a jury would likely be very sympathetic to a grieving mother who lost her baby. I think this lawsuit will probably settle before trial.
Previous Cases: