A 46-year-old woman called her primary care office with a cough and shortness of breath.
She had been seen at this clinic for years by 2 physicians and a PA.
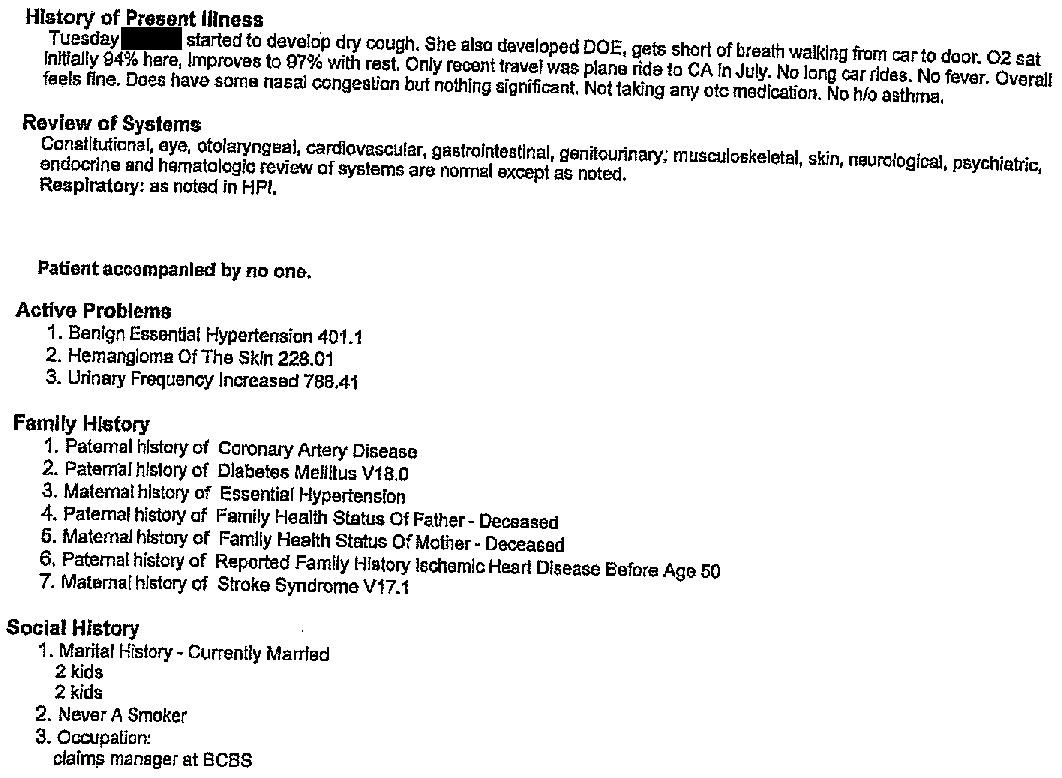
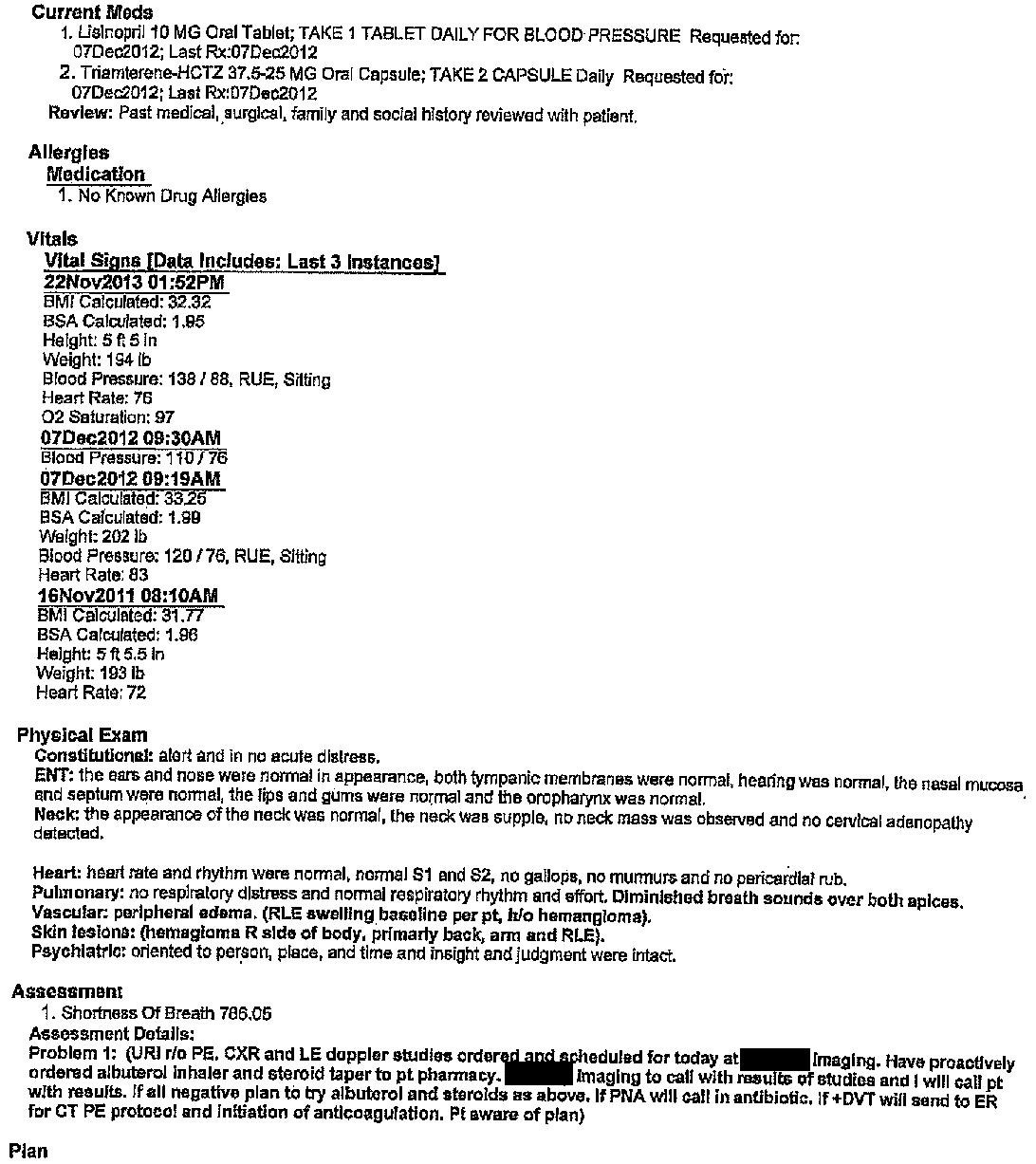
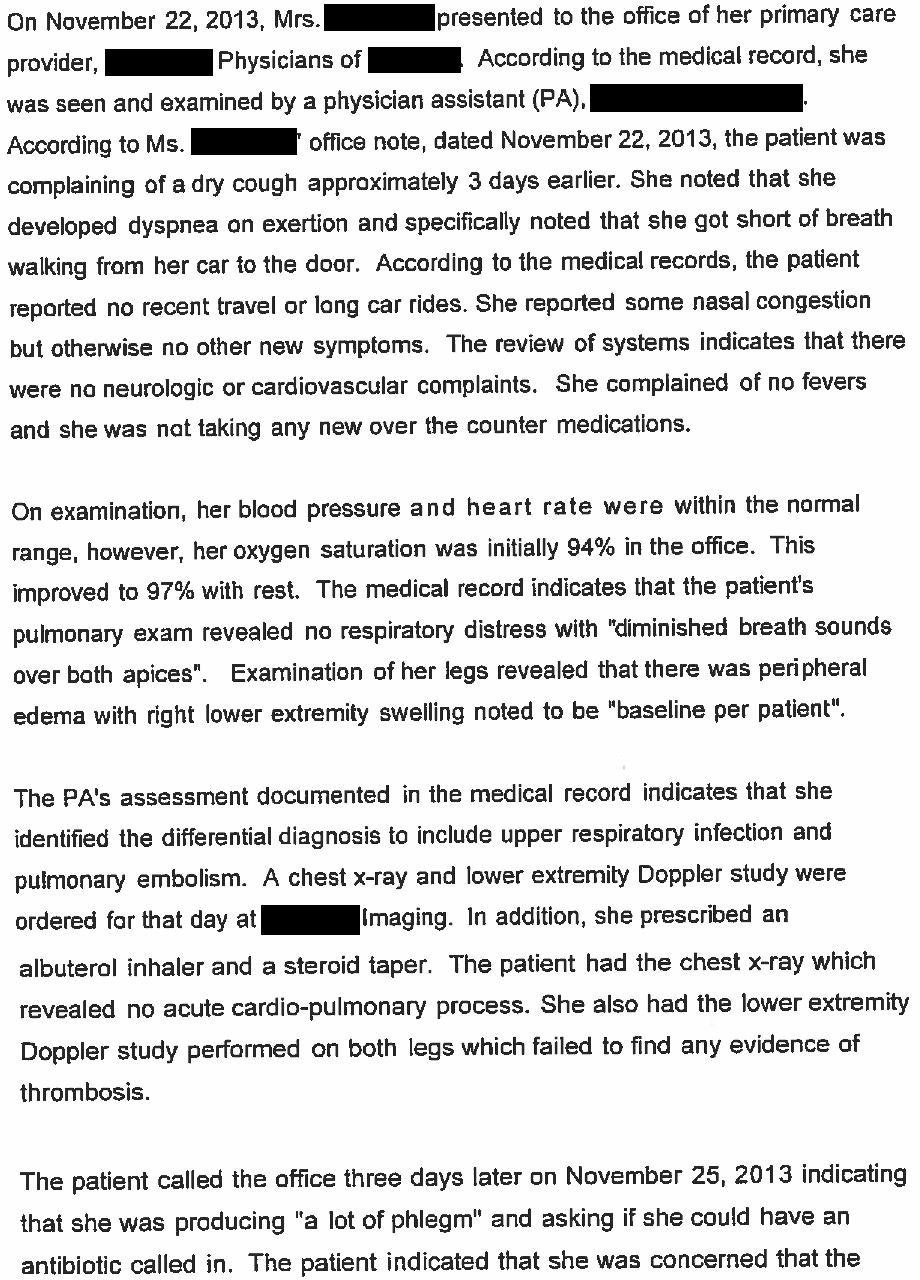
She came in for an appointment and was seen by the PA.
Her vital signs were normal.
Her initial oxygen saturation was 94%, and on recheck was 97%.
The PA documented a differential including upper respiratory infection and pulmonary embolism.
She ordered a chest x-ray and ultrasound of both legs.
The patient was given an albuterol inhaler and steroids.
The medical record (actual exhibit from the lawsuit) is shown here:
The results of the chest x-ray and ultrasounds were both negative for any acute process.
3 days later, she called and reported that she had worsening phlegm production.
A Z-pak was prescribed.
Join 6600+ doctors and lawyers.
Paying subscribers get a new case every week.
Within 24 hours, the patient had collapsed and was taken to an academic medical center.
She was diagnosed with a saddle PE, basilar artery occlusion and right carotid artery occlusion.
She had a long hospital course and slowly declined despite numerous aggressive interventions including a craniectomy.
She died 3 weeks after her initial visit.
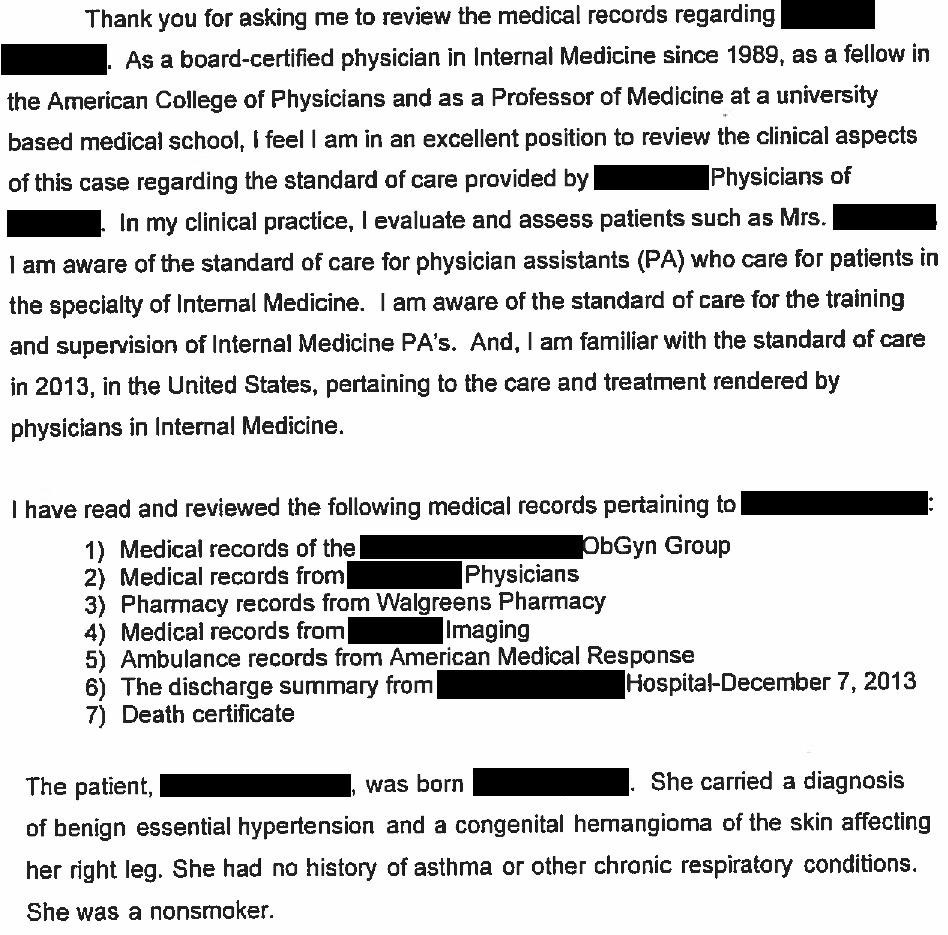
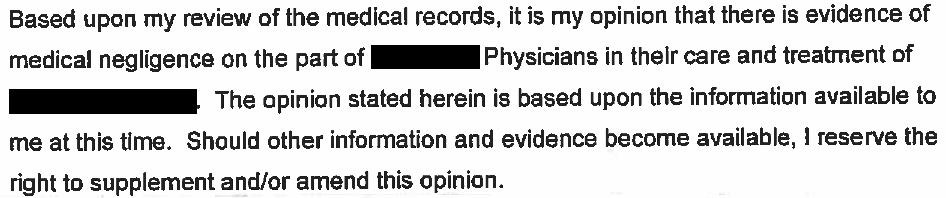
During the patient’s hospital stay, the doctors discovered that she had an underlying condition that increased her likelihood of thromboembolic disease.
Challenge question: What condition did this patient have?
If you need a hint, review the physical exam in the note above.
If you need another hint, check out this statement from the patient’s husband, who gave a deposition for the lawsuit:
Scroll to the very bottom of this post for the link to the answer. No cheating!
Here’s what other physicians are saying:
"Thanks for all the work you do in putting these together. Always so interesting to look at cases and see how things unfold. The cases also make great teaching points for the residents on rounds." - Dr. Emily Rushing
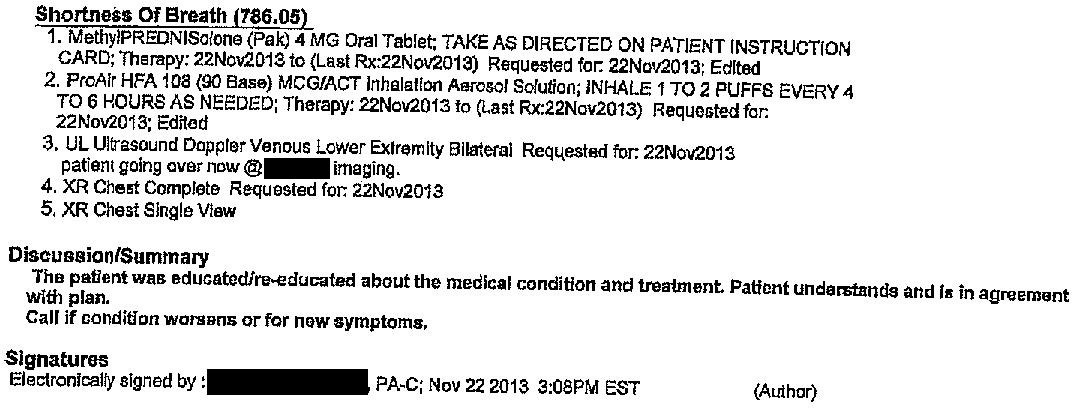
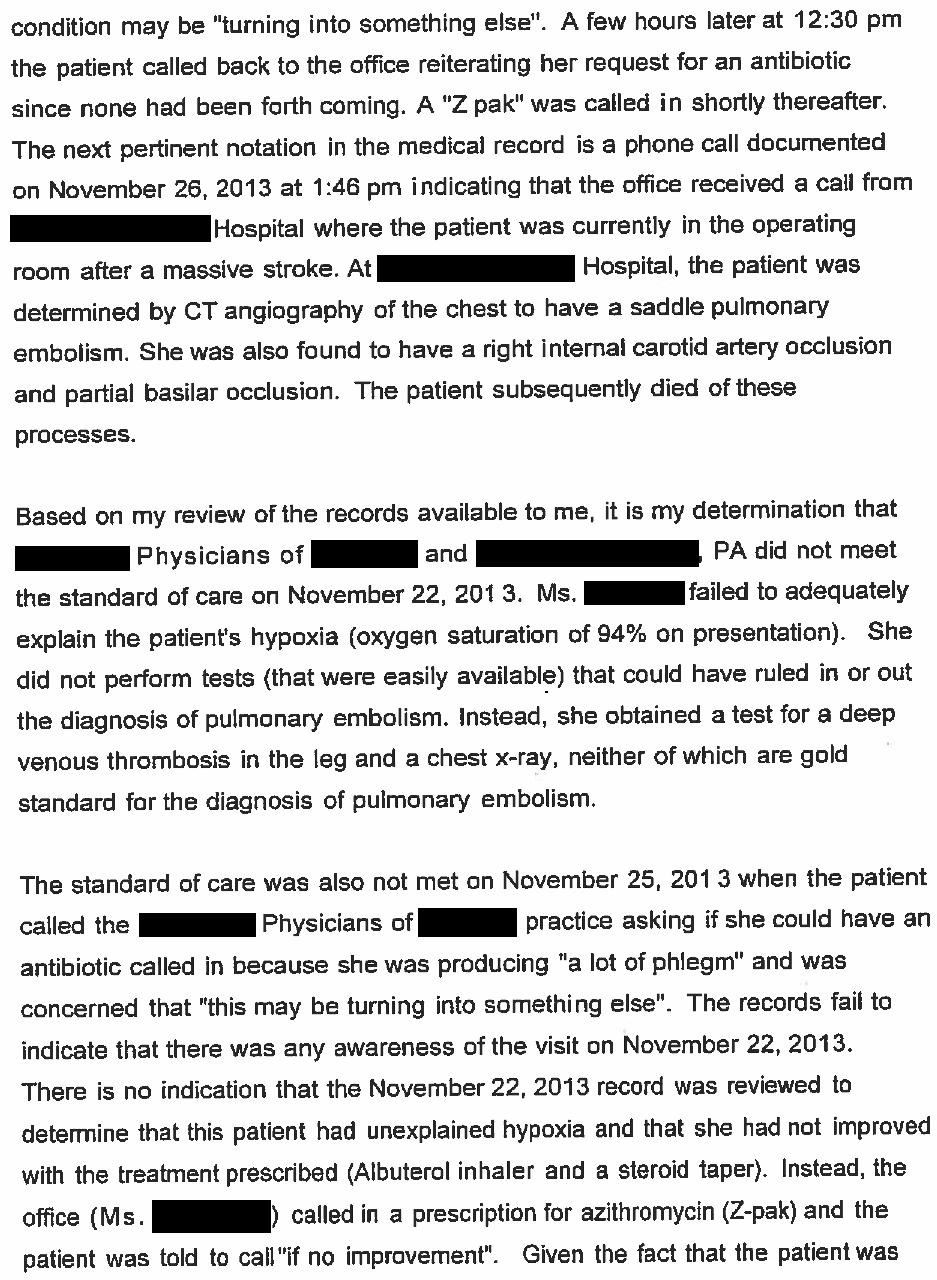
After her death, the patient’s family contacted a law firm.
An expert witness was hired and wrote this opinion:
The lawsuit was filed in February 2016 (more than 2 years after the patient’s death).
The defense never submitted any of their own expert opinions.
The case dragged on for 5 years, and reached a confidential settlement in July 2021.
MedMalReviewer Analysis:
This case is a slam dunk for the plaintiff. The PA documented that she was concerned for a PE and then failed to test the patient for a PE. This failure cost the patient her life and (likely) her employer’s insurance millions of dollars.
The expert’s claim that an oxygen saturation of 94% is hypoxic is objectively incorrect. This is another example of an expert overreaching on their criticism. There are numerous valid criticisms in this case, there was no need for the expert to ruin their credibility by making the hypoxia claim.
The 2 physicians who had previously seen the patient were also named as defendants in the lawsuit, despite not being involved in the patient’s care at her final visit. They never made any attempt to directly review the PA’s care. They were sued for inappropriate supervision and not having diagnosed the patient’s underlying medical condition that increased her likelihood of thrombembolic disease.
To see the final diagnosis and more information from the case, click here:






My thought was that the PA considered a PE because the respiratory symptoms plus a possible DVT (swollen leg). If the leg wasn’t swollen, then the consideration of PE likely would not have been mentioned. I don’t think this is a slam dunk
My first thought is this would have passed the PERC rule. But, in fact it wouldnt have. Sat of 94% screens positive for PERC. An ER doc would have done a D-dimer, but of course the setting is different in a primary care clinic than an ER - the needle is hiding in a much bigger haystack in primary care than in the ER.