A 69-year-old man was diagnosed with prostate cancer and seen by a urologist.
A robotic-assisted prostatectomy was recommended.
Following the procedure, he developed worsening abdominal pain and sepsis.
He was ultimately diagnosed with a bowel injury.
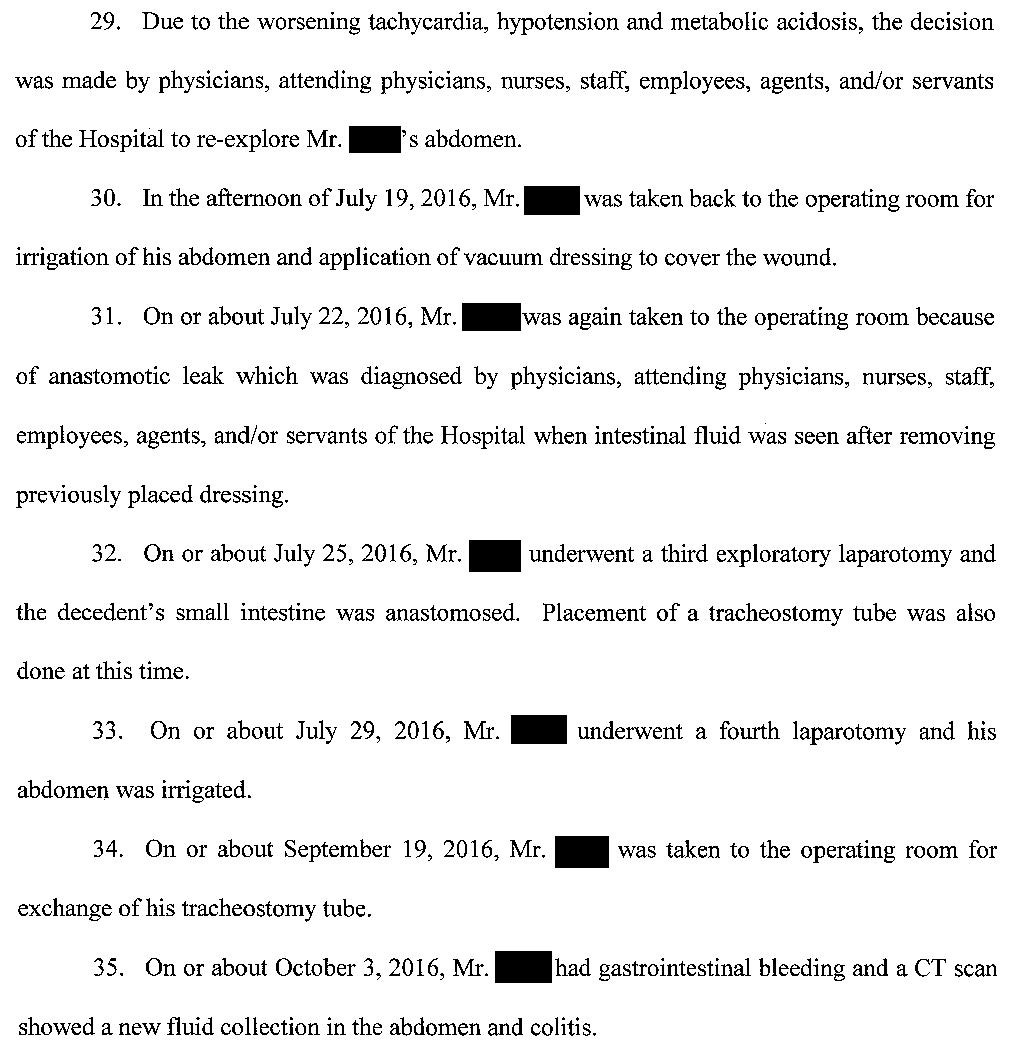
Over the following months he was taken back to the OR multiple times.
He ultimately died 4 months later of complications.
Join 7800+ doctors and attorneys on the email list.
The events following the surgery are described here by the plaintiff.
The patient’s wife has sued the hospital, the urologist who did the surgery, as well as a separate urologist who reassessed him while he was on call.
The plaintiff hired a urology expert witness.
The plaintiff’s attorney demanded the urologist’s personnel file from the hospital, including any disciplinary records.
The hospital refused to produce this, and they were not compelled to do so by the judge.
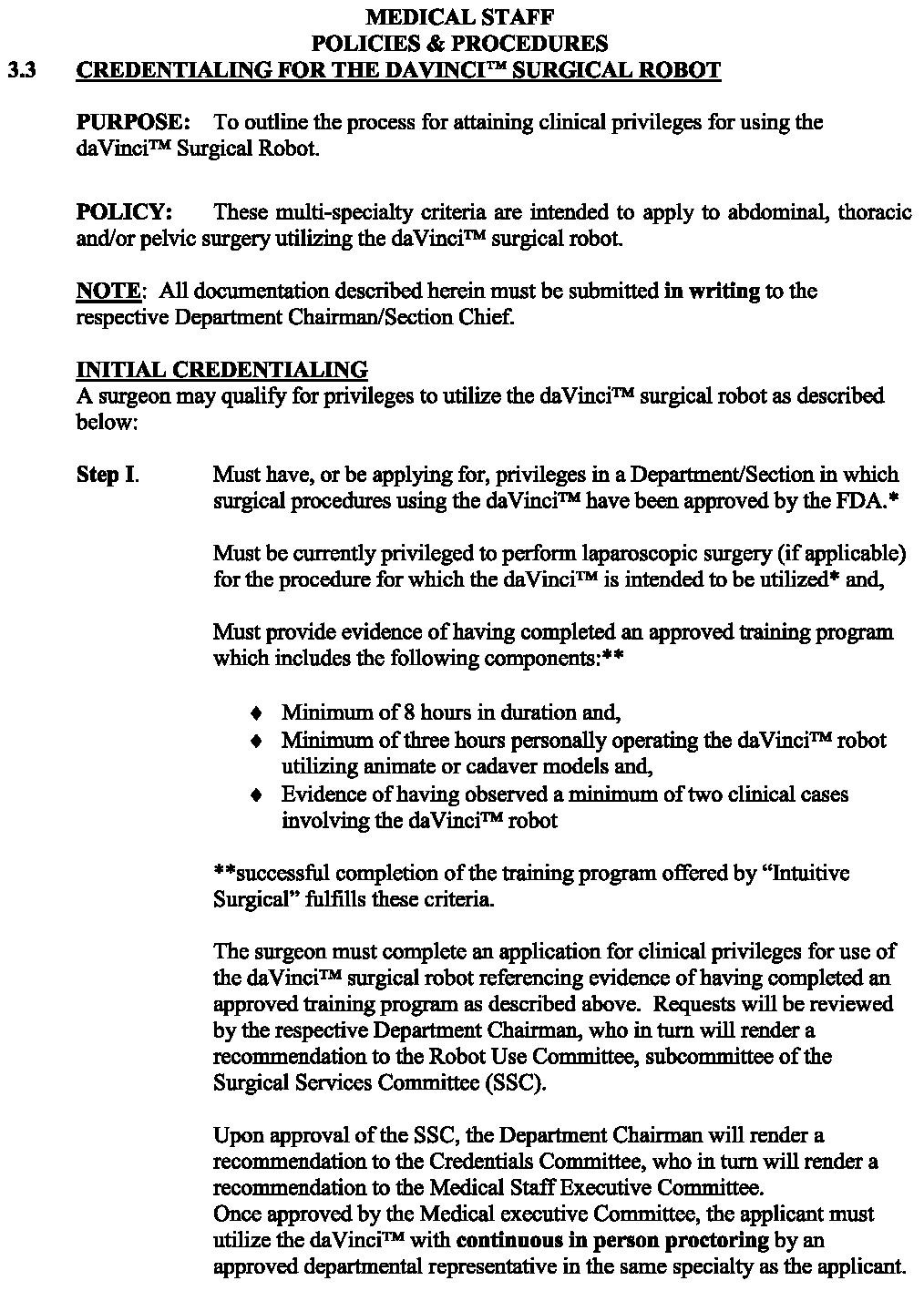
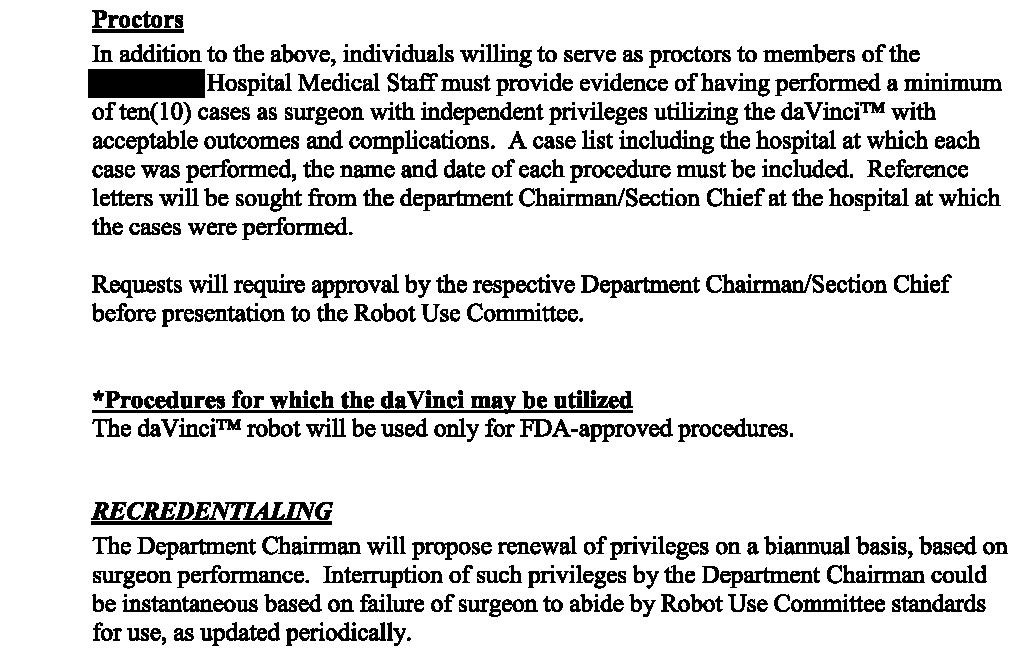
They also requested the hospital’s policy on robotic surgery credentialing, which is shown here:
Avoid the pain of a medical malpractice lawsuit.
Pick up a paid subscription today to improve your medicolegal expertise and gain valuable clinical insights that are difficult to find anywhere else.
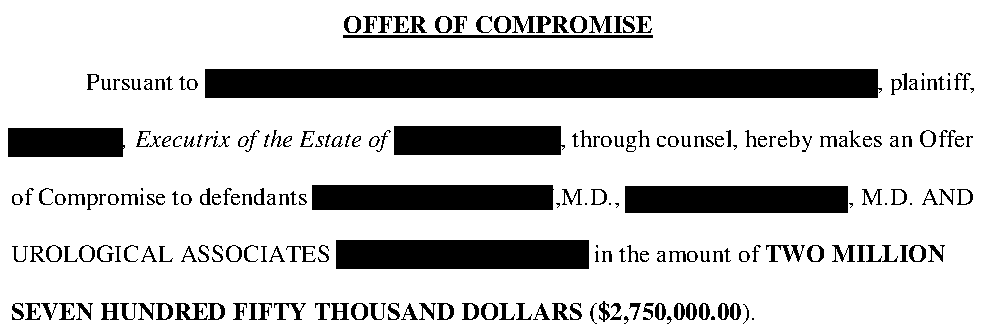
The plaintiff has offered to settle with both urologists for $2.75 million.
The hospital reached a confidential settlement after an initial offer of $5 million.
The lawsuit is still ongoing.
MedMalReviewer Analysis:
This expert opinion lacks any substantial claims of how the urologist was actually negligent. They simply identified a bad medical outcome and are working backward to make up vague claims of negligence. A bad medical outcome alone does not prove negligence.
Furthermore, it is painfully clear that the expert did not actually write this opinion. The plaintiff’s attorney wrote it, then shopped around until he found a urologist who was willing to sign their name to it for the right price. There is no medical discussion of the case, simply a regurgitation of legal talking points.
The credentialing policy for using the robot seems relatively lax, requiring only 8 hours of training. If you use a DaVinci robot in your practice, is this a standard credentialing policy?
Previous Cases:






If the physician who signed this expert witness opinion is an academic, it sets a poor example for residents and trainees. The opinion is so vague and lacking in substance that it should be reviewed by the AUA, which has established guidelines for expert witness testimony. While it is unfortunate that the events of the case led to the death of the patient, it is challenging to reach any meaningful conclusion without knowing the details of the patient’s general condition and postoperative course. Poor outcomes can occur in complex cases despite appropriate care, but a clear breach of the standard of care must be demonstrated for a malpractice claim to be valid. This opinion fails to do so and instead appears to be more of a legal maneuver than a genuine medical evaluation.
Bear in mind that to get training to use the robot, you have to already be competent in that particular procedure laparoscopically. If you don't know how to do the procedure, you wouldn't get those privileges. The training for the robot is to learn how to do the procedure you already know how to do with a different instrument, the robot. Robotic training does not teach you how to do surgery, only how to use the robot to do the surgery. The length of training should not have a bearing in the case unless the injury was somehow caused by some malfunction or misuse of the robot or robotic instruments. I agree that they are trying to manufacture a case of negligence based on a bad outcome.