A 36-year-old man developed vomiting, diarrhea, and a fever.
He was diagnosed with trichothiodystrophy as a child and had intellectual impairment.
He had undergone surgery on a heart valve as a child, exact details were unknown.
After several weeks of lingering symptoms, he presented to a nearby ED on July 6.
In addition to vomiting and diarrhea, he also reported shortness of breath as a secondary symptom.
A chest x-ray revealed cardiomegaly and a possible lung infiltrate.
CBC and CMP did not show any worrisome findings.
He was discharged on antibiotics to treat suspected pneumonia.
On July 12 (6 days after the initial ED visit) he presented to his PCP’s office.
He previously had been seen by the physician, this time he was seen by an NP.
She noted that antibiotics “didn’t help his sweating, diarrhea, or vomiting”.
She repeated a chest x-ray, showing only cardiomegaly.
The infiltrate had resolved, so she did not continue his antibiotics.
She diagnosed him with a viral syndrome and advised PO fluids and rest.
He returned on July 18 with similar complaints.
He saw the same NP and was given similar advice.
A 3rd visit with the NP occurred on July 22.
He described vomiting, abdominal discomfort, a “puffy” abdomen, and decreased urination.
His mother accompanied him on this visit, and reported he was sweaty and short of breath at times.
Labs were repeated.
The only noteworthy findings were a creatinine of 1.6 (previously normal) and his AST/ALT were slightly elevated (exact numbers not given in court documents).
The same plan of care was continued.
2 days later (July 24) he returned.
He again reported abdominal distension and vomiting.
A urinalysis was done, showing bacteria. He was started on ciprofloxacin.
The NP ordered a CT of his abd/pelvis.
It was completed later that day.
The impression mentioned 5 points:
Cardiomegaly
Bilateral pleural effusions and nodular infiltrate in the right lower lobe
Ascites
Anasarca
Bilateral inguinal hernias containing fat
The radiologist called the patient’s physician to communicate these results.
The physician then called the patient’s mother, and told him to go to the ED if he was short of breath.
The following day (July 25), the patient had worsening shortness of breath.
He presented to the ED just before midnight (different facility than the initial ED visit).
The history, exam, labs, and chest x-ray were consistent with heart failure.
The patient was admitted to the hospitalist.
Diuresis was started.
He was moved from the ED to his hospital bed at 5am in the morning.
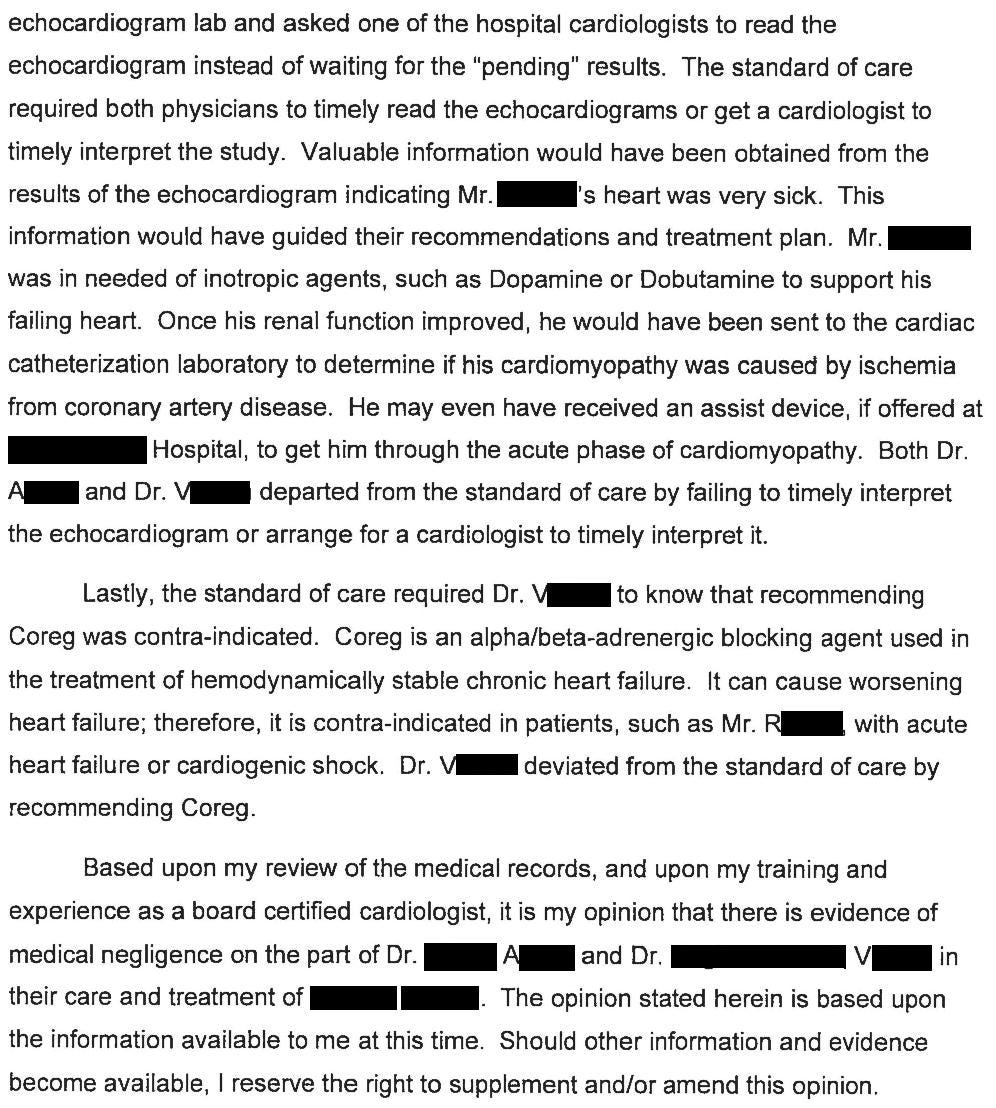
Later that day (July 26) he was seen by a cardiologist (Dr. A).
Dr. A recommended continued diuresis and ordered an echo.
The echo was completed at 12:32pm.
The echo tech later stated that she called Dr. A and advised him that the EF was severely reduced (later reported as <20%) and he had biventricular failure.
On July 27, the patient was seen by a different cardiologist (Dr. V).
He noted that the echo report was still pending.
Dr. V recommended the patient start Coreg.
The patient was given the first dose.
20 minutes later he went into cardiac arrest.
Despite attempts at resuscitation, he never had ROSC and was declared dead.
His echo was read 2 days later.
Join 11,000+ doctors and attorneys on the email list.
Free to join.
Paid options available for those who want to expand their medicolegal expertise and become a better doctor.
The patient’s parents contacted a law firm.
A lawsuit was filed against both cardiologists, the NP, and the primary care physician.
Neither ED physician, the hospitalist, nor the hospital were named as defendants.
A cardiologist was hired by the plaintiff:
The defense hired a cardiologist, subspecialized in advanced heart failure and transplant cardiology.
The attorney’s summary of his opinion is shown here:
The plaintiff hired an NP expert witness as well:
The plaintiff has offered to settle.
They are requesting $3,000,000 from each cardiologist, and $1,000,000 from the primary care physician.
There has been no offer to the NP. It’s unclear if this was intentional or an oversight.
The lawsuit is ongoing.
I’ll send updates by email when new developments happen.
Make sure you’re on the email list to be notified:
MedMalReviewer Analysis:
This case is a good opportunity to review guideline-directed medical therapy (GDMT). The defense expert briefly mentioned the phrase but didn’t go into detail. It’s also called “quadruple medical therapy” or “the 4 pillars”. If your practice involves seeing patients with heart failure and you don’t know what “GDMT” refers to, its time to get with the program. I’m not a heart failure expert and the research has progressed considerably since 2013 when this case happened, but its worth knowing that GDMT refers to a combination of 4 medications used to treat patients with HFrEF:
ARNI: angiotensin receptor/neprilysin inhibitor (ex Entresto)
Beta-blockers (ex Coreg)
MRA: mineralocorticoid receptor antagonist (ex spironolactone)
SGLT2i: sodium-glucose co-transporter 2 inhibitor (ex Jardiance)
One of the central issues is if the patient was stable enough to start Coreg. I have a hard time believing that both cardiologists would have missed decompensated heart failure that was so severe that he was on the precipice of cardiogenic shock. There’s a gradient of heart failure severity that ranges from slightly-decompensated to severely-decompensated to cardiogenic shock. The extremes are obvious, but the point on this gradient at which Coreg becomes contraindicated is not entirely clear to me.
The pharmacokinetics of Coreg are worth considering. The court documents state that the patient coded 20 minutes after receiving the medication. A brief review of the literature doesn’t give a clear answer to the rate of absorption or how long it takes for the first detectable amount in the blood. However, it takes 1-2 hours to reach peak concentration. If I was the defense, I would be tempted to hire a pharmacologist to refute the claim that Coreg caused his cardiac arrest.
Heart failure can be hard to diagnose in patients who have GI issues as their first symptom. Don’t fall prey to anchoring on GI illness just because a patient has vomiting and diarrhea. Multiple bounceback visits should cause you to broaden your differential and search for alternative explanations. In hindsight, there were other clues that this patient was in heart failure, including the shortness of breath and diaphoresis. An old adage comes to mind: “if your patient is sweating, you should be sweating too”.
This patient had a rare genetic condition called trichothiodystrophy. It’s an autosomal recessive genetic disease caused by mutations in DNA repair genes. Patients usually have brittle hair, intellectual impairment, and short stature, among other findings. Cardiac issues of various types can be seen, although the exact nature of cardiac disease seems to be quite variable. Its impossible to say with certainty, but I’m suspicious this patient’s underlying genetic disease played a role in his heart failure and death.
ER doctors: Looking for a good EM job? Tired of CMGs crushing our specialty? Check out this posting for a democratic group that works by the beach in Monterey, CA.
Looking to hire an EM doc? Click here to get in front of thousands of BC/BE EM physicians.










I don't understand why vital signs were not collected at each visit. They're painless (for the most part), non-invasive, and offer great insight into a patient's condition---especially when trended over time. It seems that vital signs don't get any respect.
One of the best journal articles I have shared with others is "Make Vital Signs Great Again." In the hospital, we have several early warning systems (NEWS, PEWS, MEWS)----but they don't work if staff don't enter the vital signs, and they're definitely not helpful when staff "batch" the vital signs after they finally have a breather at 2 in the morning. Unfortunately, when they go to draw labs at 4 in the morning, the patient is in rigor.
Speaking of carvedilol pharmacokinetics, one point that isn't mentioned is it's metabolism is mostly hepatic and there is a large amount of first pass metabolism so it's possible that in someone with severe liver dysfunction (which it sounds like he may have had depending on how high the INR was) you can have supratherapeutic levels even if it was otherwise indicated