A 60-year-old woman developed back pain and was referred to a neurosurgeon.
Surgery was recommended and was scheduled for January 16, 2014.
After 4 days in the hospital, she was discharged to a rehab facility.
She developed shortness of breath and was re-admitted to the hospital on January 27, 2014.
Workup revealed pneumonia and a non-occlusive DVT in her left tibial vein.
The hospitalist started her on warfarin with a Lovenox bridge.
The patient was discharged from the hospital on January 30, 2014.
A referral was made to a home healthcare agency.
They saw her several days later and a repeat INR was done on February 4, 2014.
Her INR was 2.8.
The home nurse contacted the patient’s PCP office, and a nurse practitioner advised to stop taking the Lovenox.
The following day the patient developed severe back pain and new-onset incontinence of bladder and bowel.
She was taken back to the hospital.
Imaging revealed a large spinal hematoma at the operative site causing cauda equina syndrome.
She was taken to surgery but suffered permanent weakness in both legs.
Join thousands of doctors and attorneys on the email list.
The patient contacted a law firm and a lawsuit was filed.
They sued the hospitalist who discharged her on the anticoagulation bridge, and the home healthcare agency for not checking her INR soon enough.
They did not sue the neurosurgeon.
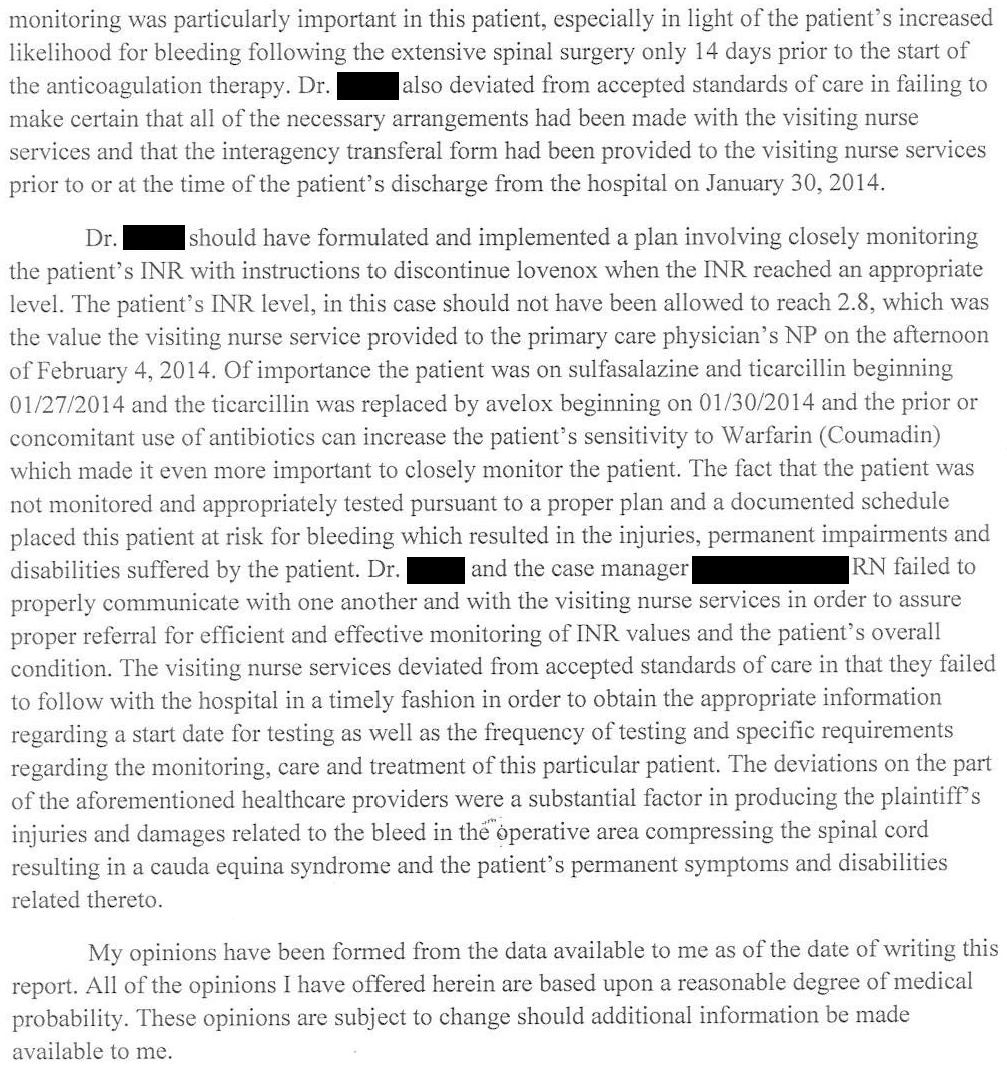
An expert witness was hired and wrote the following opinion:
The case was settled for a confidential amount.
Subscribe today to get access to weekly cases and the entire case archive.
Grow your medicolegal expertise through consistent case review.
MedMalReviewer Analysis:
The attorney focused heavily on the fact that there was a multi-day gap between discharge and the home healthcare agency checking her INR. He is eager to blame the doctor for this, but in reality the hospital social worker and the home healthcare agency are responsible for the logistics of arranging this.
The patient never had a supratherapeutic INR. It was at an appropriate level and the Lovenox had already been stopped when she developed cauda equina syndrome. This lawsuit seems to stretch the bounds of reasonable criticism.
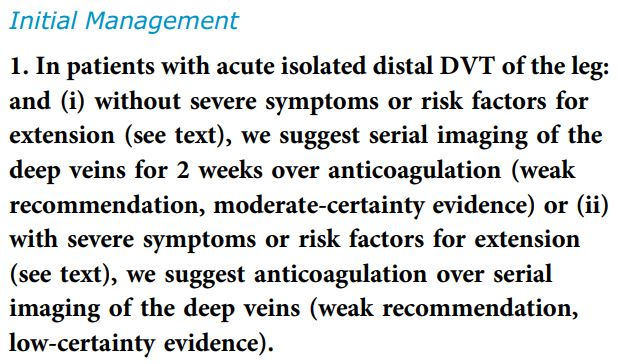
There is an interesting conversation to be had about the utility of starting anticoagulation in patients with distal DVTs. The risk of PE from these distal DVTs is much smaller than proximal DVTs.
The best guidance on this issues comes from Chest, which most recently released guidelines in August 2021.
Those who want to read more can review the guidelines on page 2 of this PDF, with more detailed information on page 9.A few questions for those who manage DVTs and bridge anticoagulation:
How often do you check an INR during the bridge?
At what INR do you stop Lovenox?
What percentage of isolated distal DVTs do you anticoagulate and what percentage do you order serial imaging?
Anticoagulation complications are a common source of malpractice lawsuits. This prior case [Subscriber Content] involved a head bleed caused by using a heparin drip in a patient who already had an INR of 5.6:
In another prior case, a patient had a spontaneous epidural hematoma that was missed initially. The hematoma was located in the thoracic spine after negative lumbar imaging, a pattern that I’ve noticed in multiple lawsuits.
Last week’s case for subscribers was about a patient with coronary artery disease who was switched from clopidogrel to prasugrel despite a history of stroke and black box warning for this issue. He suffered a large hemorrhagic stroke.






I think this particular question is moot. The only pts. who receive warfarin now have a metallic valve replacement; an intracardiac thrombus; a NOAC failure; or a preference for warfarin (price, etc). The DVT's I treat in the ER get apixaban/ rivaroxaban/ etc. Discount cards that provide the first month of treatment for free are plentiful. Even pts. with a PE (who meet guideline requirements for outpatient management) receive one of the newer medications, over a "bridge" of enoxaparin and warfarin.
This has been my recent experience.
I love how the complaint says the INR reached a "therapeutic range of 2.0."
A range ... of one specific number.
Is this just moronically sloppy writing, or is the attorney trying to distract from the fact that the therapeutic range for INR is 2.0-3.0?
This is the kind of crap that drives me nuts.