A case I first published over 2 years ago has now settled.
Here’s the brief summary:
A 60-year-old woman presented to the ED with vomiting.
She was diagnosed with DKA and admitted.
The next day she developed excruciating (10/10) right leg pain, numbness in her toes, leg weakness, and her leg was cool to the touch.
For some reason, the medicine team did not react with any urgency.
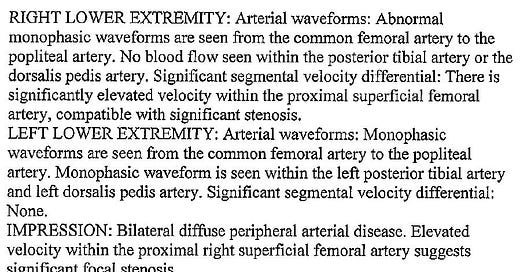
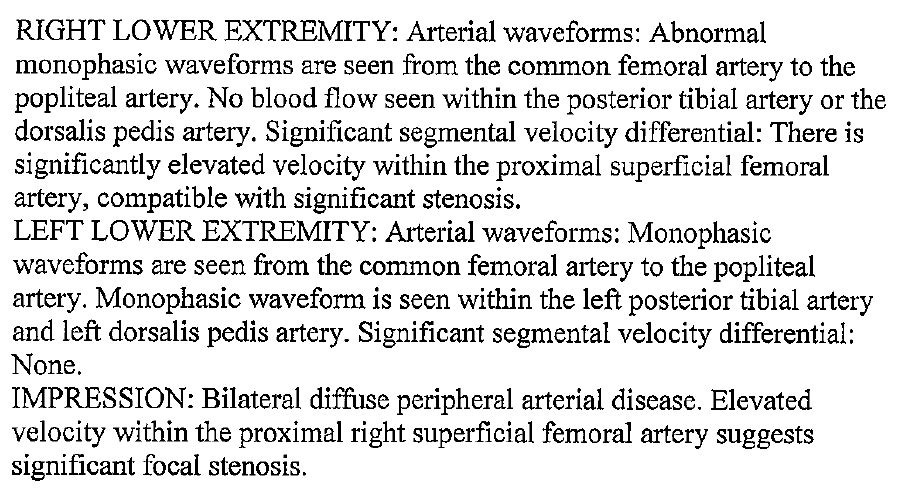
They ordered an ultrasound:
They “considered” a vascular surgery consult.
But they didn’t consult vascular surgery.
A new team of residents started the next day.
They realized something was wrong, and consulted vascular.
She had a large femoral artery clot and her leg was amputated.
The hospital and doctors have now reached a settlement.
Subscribe to get a new case every week!
This week’s case revolves around a post-op sigmoid resection in which an FM-trained hospitalist kept treating tachycardia and delirium with CIWA protocol and beta blockers.
Only problem is that they weren’t actually in alcohol withdrawal.
It’ll be published in a few hours.
Another topic I wrote about this week:
The most underrated question to ask when interviewing for an EM job.
I’d be curious to hear your opinion on this article! Send me a reply.