Editors note: I received this case via anonymous tip and it blew me away.
It’s probably the longest case I’ve ever written, but I think its worth the read.
A healthy, fully-vaccinated 7-year-old boy presented to the ED in the middle of the night during February 2020.
The nurse triage note stated “woke up sob. felt warm so he got motrin pta. says his sob feels better.”
Triage vitals were taken:
Temp: 39.4C
HR: 135bpm
RR: 26/min
Pulse ox: 95%
He was roomed and seen by a PA, with direct supervision by a board-certified EM physician.
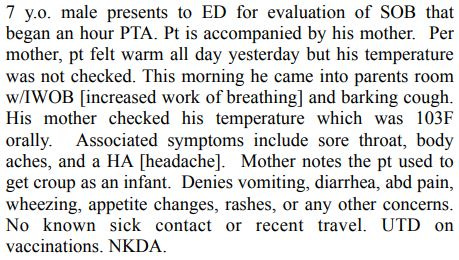
The PA documented the following history:
The only positives on the physical exam were mild nasal congestion and a “barky” cough.
The remainder of the respiratory exam was normal.
The PA ordered PO dexamethasone and a viral PCR swab for RSV and influenza.
The PCR swab came back positive for influenza B.
The child’s temperature was re-checked and was 99.5F.
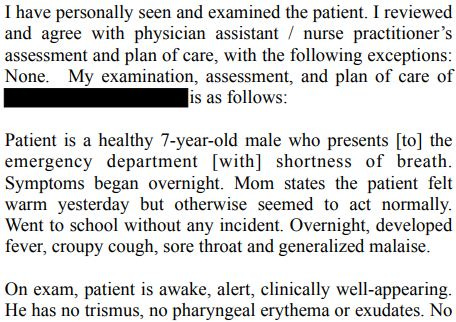
The ED physician personally evaluated the child and discussed the results and treatment options with his mother.
The supervisory note is here:
The child was in the ED from 4:42am to 6:15am.
Before reading the outcome, please answer the poll:
During the following 36 hours, he continued to have malaise and fever.
At around 7pm the next day, he was sitting on his mother’s lap.
He told her he was having problems breathing, then collapsed in cardiac arrest.
EMS placed an IO and coded him at home.
They briefly got ROSC and he was intubated.
He was rushed back to the same ED, where he coded again.
Tragically, he could not be resuscitated and was declared dead.
The following day, an autopsy was done.
The cause of death was “influenza B infection and necrotizing pneumonia”.
Blood cultures drawn in the ED were positive for Group A Streptococcus (GAS).
Join 8900+ doctors and lawyers on the email list.
Free and paid options available.
A lawsuit was filed against the doctor, the PA, and the hospital.
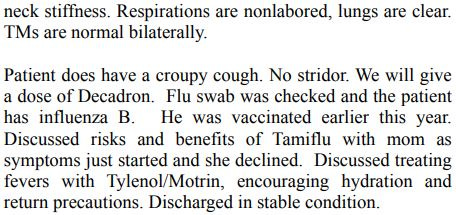
Part of the allegations against the defendants are shown here:
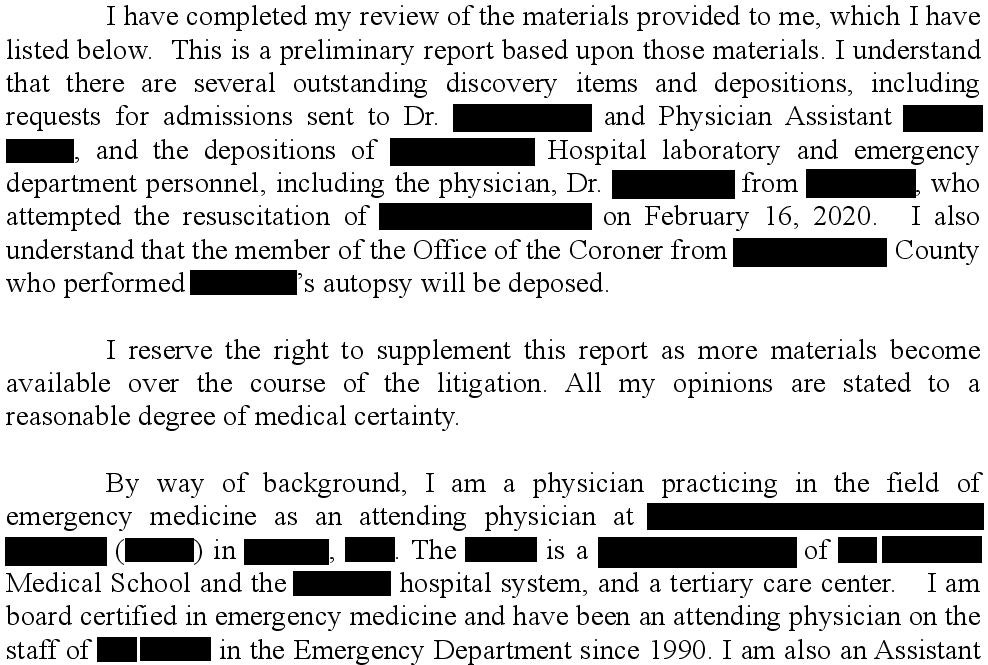
An expert witness was hired.
He completed an IM residency but was boarded in EM.
He practices in a large academic medical center with an EM residency.
All parties reached a confidential settlement.
MedMalReviewer Analysis:
It would be a mistake to start my analysis of this lawsuit without acknowledging the tragedy of this case. As both a father and an EM physician, this is absolutely my worst nightmare. I can’t begin to imagine the grief felt by his parents as he collapsed in their arms and died. My heart truly goes out to them.
The expert in this case claims that the care provided was “shocking and outrageous”. My opinion is quite the opposite. The physician and PA were diligent and treated the child appropriately given the information that they had. The only thing that I find “reckless, shocking and outrageous” is this expert’s opinion.
Let’s look through each of the expert’s points:
Inappropriately diagnosed and treated for croup. Croup is simply a manifestation of upper airway swelling that can lead to inspiratory stridor and barking cough. There are numerous potential causes of croup, both bacterial and viral. While parainfluenza is the most common, influenza is also well known to cause croup. The expert is incorrect in implying that influenza B and croup are mutually exclusive diagnoses.
The expert also points out that the child was 7-years-old, above the normal croup age range. While I agree that this should raise concern, I don’t think it was an entirely unreasonable diagnosis in light of a barking cough, respiratory illness, history of croup, and overall benign clinical appearance.
Croup is a clinical diagnosis, not an autopsy diagnosis. A pathologist may be qualified to comment on the gross pathology findings suggestive of croup, but not an EM physician. Furthermore, this is a retrospective and useless criticism of the bedside clinicians, who would obviously not have access to their patient’s autopsy results.Giving this patient steroids to treat croup while waiting for PCR results is inappropriate. Croup is a clinical diagnosis. There is no need to wait for any test results to begin treating croup. For the sake of argument, even if they had waited for the results of the PCR test, it would still not have been contraindicated to give dexamethasone. Influenza is a well-known cause of croup.
Use of the language “reckless, shocking, and outrageous” is gratuitous and unprofessional. He seems more interested in being dramatic than communicating a rational evidence-based opinion.Decadron administration is not an approved treatment for pediatric influenza. This is correct, and the defendants knew that this was correct. They did not give steroids to treat pediatric influenza. This is an empty criticism.
Only one set of incomplete vital signs was performed. The expert attempts to claim that the lack of a blood pressure means the vital signs were incomplete. However, a joint policy statement from AAP and ACEP explicitly states “infants and children should have a full set of vital signs recorded to include temperature, heart rate, and respiratory rate”. Note that blood pressure and pulse ox are not required for a full set of vitals, and only need to be available on the basis of the child’s presentation. This presentation did not require a blood pressure. It’s interesting that the expert (an ACEP member) did not consult his own college’s guidelines while writing this opinion.
We’ve debated the value of discharge vitals in a previous pediatric influenza case. The fact that a repeat temperature was normal demonstrates appropriate diligence and frankly is what the vast majority of responsible clinicians would do in this scenario.The physician holds the PA responsible for giving Decadron. It appears that the PA gave Decadron prior to presenting to the physician. I don’t find this criticism to be warranted because the physician clearly agreed with the plan. He nitpicks the difference between using past-tense and future-tense in regards to documenting “We will give Decadron”, which has no significance.
They were never offered the opportunity to be evaluated by a pediatric specialist. Some context is important here. In this hospital, pediatric patients are seen from 7am to 11pm by either a pediatrician or PEM specialist. The patient was discharged at 6:15am. The expert seems to be suggesting that the child should have been held in the ED until 7am, or a pediatrician should have been consulted. There is simply no reason to call a consult for a 7-year-old child with a croupy cough and influenza B, who appears well, has normal oxygenation, and had documented resolution of his fever.
Furthermore, the expert’s appeals to patient autonomy are bizarre. Patient autonomy does not imply that a specialist has to be inappropriately consulted. Nor is there any reason to believe that an offer to wait to see a PEM physician would have been accepted.
Suffice it to say, I’m not impressed with this expert’s criticisms. There are a few valid points sprinkled between numerous incorrect statements and distracting claims.
I’m also concerned that this physician was selected as the expert for this case. He’s board-certified in EM but did an IM residency. His opinion left out any reference to his qualification in caring for children. How many pediatric rotations did he do as an IM resident? Does he still actively care for children, and with what frequency?
It worries me that this expert is a faculty member who teaches EM residents at a world-renowned institution. I wonder if the university is aware that he writes these opinions underneath their logo and letterhead.
It worries me that a member of ACEP and SAEM would viciously attack a colleague in this manner.
A few other topics of conversation:
Cases that involve NPs and PAs always attract a lot of attention. It’s obvious that the physician was directly involved in this patient’s care and supervising appropriately. I don’t think this outcome happened because a PA initially saw him. Most physicians would have done the same thing. The only possible influence to consider here would be an anchoring bias. If the physician had seen the patient first and mentally categorized them as “shortness of breath with a croupy cough”, it may have produced a different workup than one presented to them as “croup”. But this is purely speculative. Just be aware that anchors are heavy and can sink you.
Its worth discussing the value of obtaining a chest x-ray in this case. Generally speaking, a chest x-ray is unnecessary in croup, and unnecessary for influenza. But it could be justified in the workup for undifferentiated shortness of breath. So much of this comes down to how we mentally frame the presentation.
There’s a decent chance that the x-ray would have only shown minimal findings which could have been explained by his positive influenza test. Even with signs of bacterial pneumonia, he might have been discharged home on antibiotics in light of his benign clinical appearance and vitals. There’s also a reasonable chance that he did not have a superimposed bacterial infection when he was seen in the ED.Invasive Group A Streptococcal (iGAS) infection superimposed on influenza is a well-known recipe for disaster. There have been public health warnings the past few months about increasing iGAS prevalence as we go through a seasonal spike in influenza cases. I’ve heard numerous anecdotal reports from other physicians about similar cases.
Learning Pearls:
The standard age for croup is 6 months - 6 years.
Not all barking coughs are croup.
Keep iGAS in mind, especially for flu patients.
It’s fine to work as an expert witness, but stick to your area of expertise and don’t make ridiculous claims.
Not all tragedies are avoidable.
Facebook blocks this newsletter from being shared on their platform.
However, this link still works: https://substack.com/profile/9224497-med-mal-reviewer
If you feel inspired, I’d appreciate you sharing it with colleagues!
If you made it to the end and still want more cases, check these out:






That "expert" opinion is terrifying. At what point do you just name and shame them on this page? They do not sound like they have any idea what they are doing, or if they do, they are lying to the court by writing these false statements. I agree with your analysis! Flu and croup are not mutually exclusive; flu can cause croup. While I don't treat children, steroids are a common treatment for bronchitis and other respiratory infections and it seemed wholly appropriate to treat empirically for steroids regardless of the eventual respiratory panel result. The criticism that a subspecialist should have been called is frankly bizarre. The treatment completely fit the presentation; a second set of eyeballs does not mean the care is better, even if they're attached to a subspecialist. Should I start consulting Pulmonary every time I see someone with a virus? After all, if that person died of an unforseeable complication, the family could say that if I had offered a Pulm consult, they would have accepted, and thus through some tortured logic, the pulmonologist would have saved their family member's life! It is so frustrating that the defendents settled and just reflects the sheer dysfunction in our medicolegal system. I am honestly grossed out by this expert opinion. It made me feel unclean to read it, it was so sleazy.
This report is unequivocally unethical. Anyone who disagrees is simply, matter of factly, wrong. I will never be convinced otherwise. Submit it to all member professional societies for testimonial peer review. Submit to the licensing state board for review. That’s the only way to rid medicine of these unethical practitioners.