Influenza Malpractice [Massive Verdict Against PA]
Case #245
A 48-year-old man presented to an urgent care with fever, malaise, fatigue, and dizziness.
He was seen by a PA (Ms. C).
It was February 2017, during a surge in influenza cases.
The PA ordered a rapid influenza test, which came back negative.
She felt his symptoms to be consistent with influenza, and given the elevated community prevalence, decided it was a false negative test.
She diagnosed him with influenza and prescribed Tamiflu.
The entire visit lasted about 20 minutes.
After discharge, the patient’s wife alleged that he was unable to walk back to the car.
A tech from the clinic used a gait belt to lift him into the wheelchair.
He was helped into a car and his wife drove him home.
Over the next few days, his fever continued and his condition worsened.
His wife eventually noticed that he was extremely confused and was not responding appropriately.
She called 911 and he was taken to a nearby emergency department.
We’ve now passed 20,000 subscribers on the email list!
If you’re not a subscriber yet, you can fix that now:
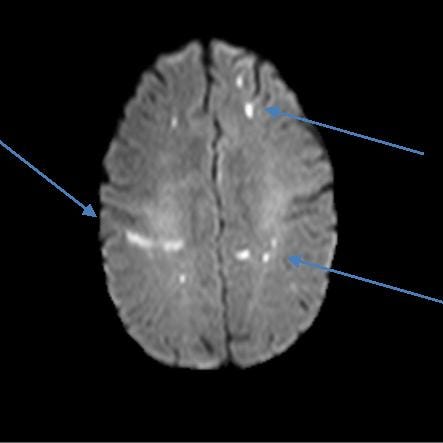
3 MRI images were included in the court records, demonstrating his stroke.
The patient and his wife contacted a law firm.
A case was filed against the urgent care, the PA, and the medical group.
The plaintiffs hired multiple expert witnesses.
The only expert witness opinion included in the court records was from a neurologist:
The plaintiff reported that the defense offered to settle for $250,000.
The plaintiff refused this settlement offer, and the defense refused to make a higher offer.
The lawsuit went to trial.
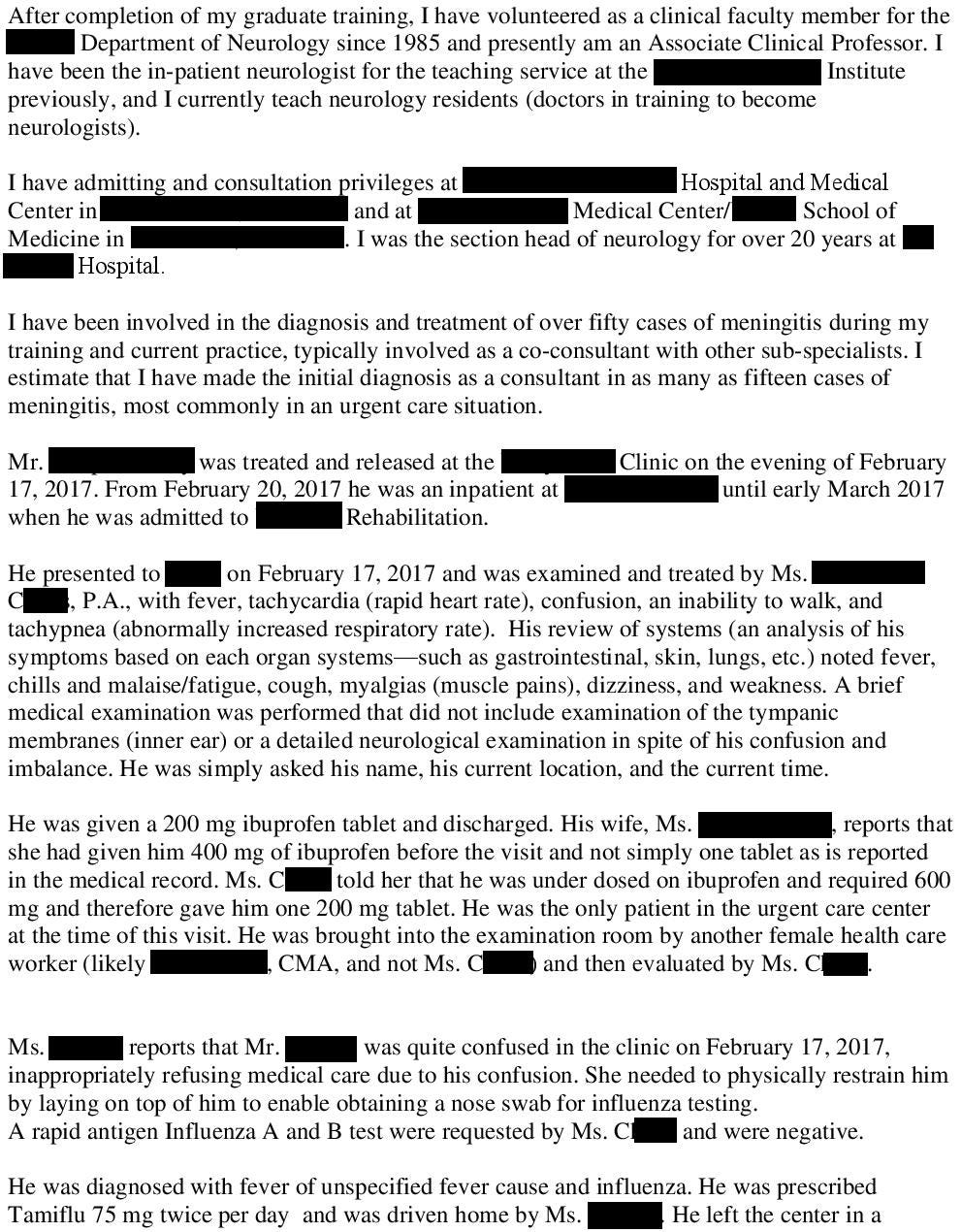
While the jury was deliberating, they sent the following message to the judge:
The judge wrote the following response:
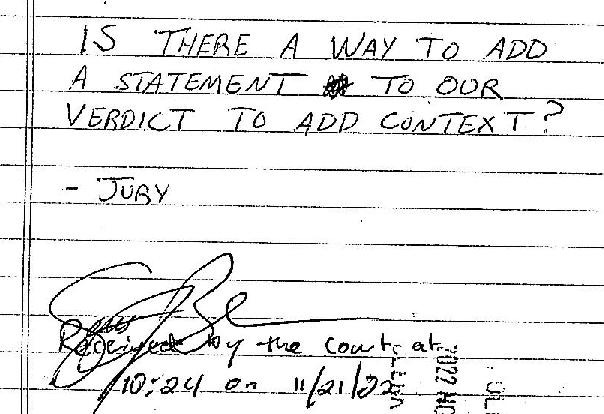
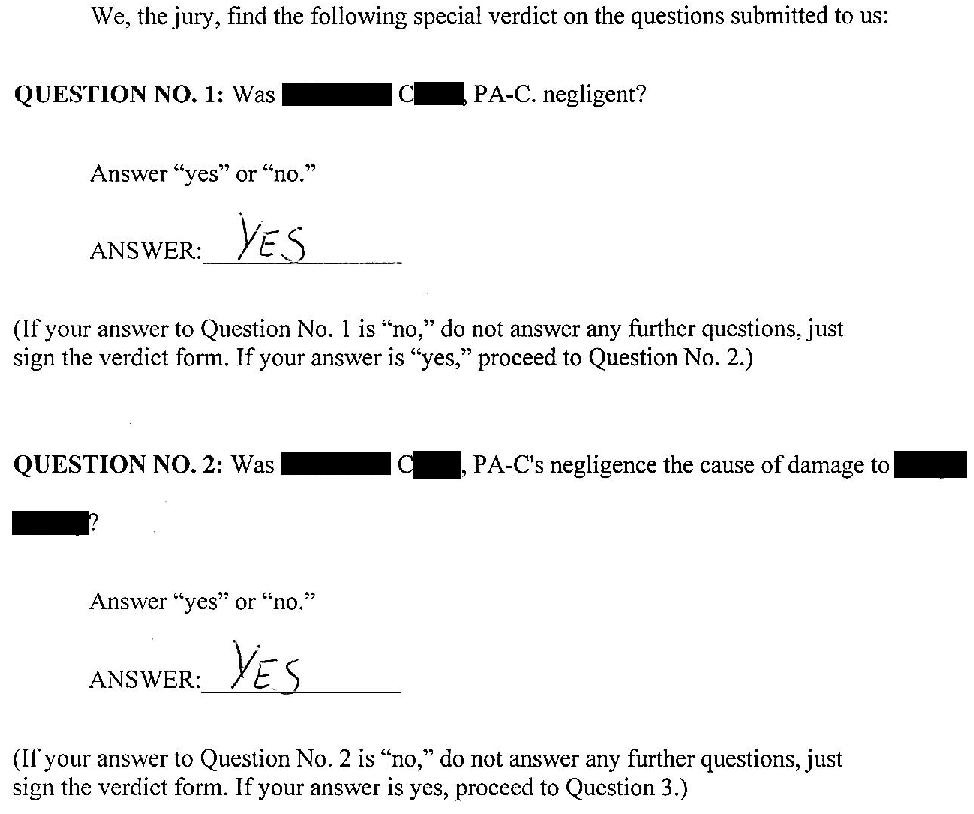
The jury returned the following verdict against the PA:
Become a better doctor by reviewing malpractice cases.
Learn from other people’s lawsuits to help avoid common pitfalls.
Paying subscribers get a new case every week and access to the entire archive.
MedMalReviewer Analysis:
This is a catastrophically bad verdict for the PA. Even more concerning is the fact that the urgent care is not listed on the verdict form. I’m guessing that the urgent care settled before trial, and the PA was left as the sole defendant. If I was being sued and the corporate defendants all settled and left me as the only defendant, I would be sending my insurer a letter demanding they settle on my behalf. Everyone knows that the PA will never be able to pay a >$20 million verdict so they’ll likely reach a resolution for a much smaller amount. But that won’t stop the plaintiff’s attorney from hitting the news circuit to flaunt their massive win and help drum up additional business.
The decision to diagnose this patient with influenza despite a negative test is very suspicious. Granted, it was a rapid test and false negatives certainly can happen. I think the overwhelming community prevalence likely swayed the PA’s decision-making. The plaintiff claimed that this happened just before the urgent care closed, which may have influenced the PA to rush through the patient’s care. The fact that this happened in an urgent care also likely caused some bias, given that patients are automatically assumed to not be seriously ill and there is significant pressure to only do very limited workups and discharge patients as quickly as possible. I really fear working in urgent care / minor case / fast track because the environment predisposes us to missing emergencies.
If it’s true that the patient was very confused and couldn’t walk on his own, then discharging him was negligent. It’s not clear if the PA realized this after the quick examination. Patients with influenza can present like this at times, so I think it was fine to start with just a rapid flu test. But once he had a negative test result, it was time to broaden the workup or send the patient to the ED.
The neurologist’s expert witness report is inaccurate at a few points. The only things he included on his post-hoc differential are sepsis and meningitis, which is a woefully incomplete differential. Numerous other infectious sources would be on the differential as well, and a true academic could dream up multiple non-infectious causes as well. He also claims that “sepsis” is bacteremia, which is a very basic misunderstanding for someone who claims to be an expert physician (even senior medical students should be able to describe the difference between sepsis and bacteremia). The plaintiff had multiple other experts that hopefully corrected these basic errors, but they weren’t included in the public court records.
I’ve been saving this case for nearly a year, waiting to publish it until influenza season for maximum impact. I’ve covered 2 other influenza cases, both were in children. One of them decompensated from the flu and was put on ECMO, surviving but with significant disability. The other developed superimposed Group A Strep pneumonia, went into cardiac arrest at home, and died. These cases are a reminder to stay vigilant during influenza season for other infections that might be masquerading as the flu, and also to stay wary about sudden decompensation of influenza patients who are showing no signs of critical illness when they’re discharged. We’ll never be able to prevent all of these bad outcomes even with excellent care, but it’s important to stay mentally alert and not get lulled into a sense of complacency amongst the sea of viral respiratory illnesses.





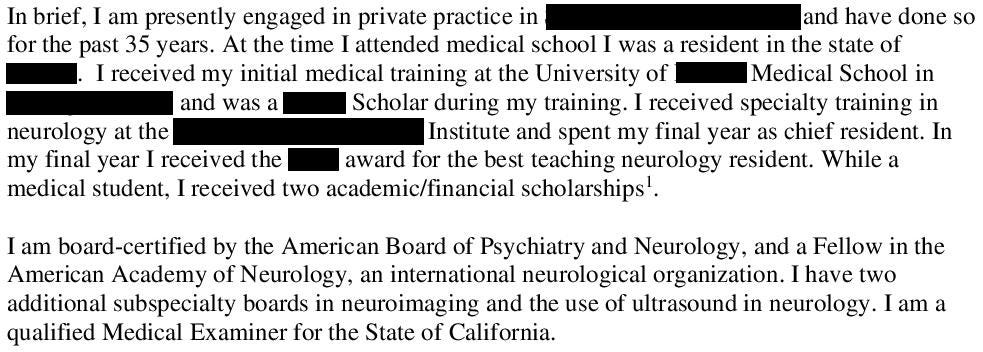




Discharging a patient with that set of vital signs and confusion (apparently severe enough that he was refusing medical care and needed to be restrained to have the nasal swab) is definitely negligent. This patient definitely needed to be referred to the ER, preferably via ambulance. A sepsis alert with an initial dose of Ceftriaxone would have helped this man tremendously.
Old adage is that fever and AMS or other neurologic findings demands an LP. We don’t always follow this in practice because determining baseline is difficult. This case is a great reminder to be diligent in these settings.
That being said, a good portion of the patients on any single day in the ICU were at an urgent care a few days prior and left with a misdiagnosis.
Urgent care is tough work.