A 48-year-old woman presented to the ED with a severe headache.
CT scans revealed a ruptured intracranial aneurysm with hemorrhage.
She had a complicated medical history and was on Coumadin (for atrial fibrillation), Cymbalta, Flexeril, Clinoril, and Lyrica.
Neurosurgical intervention was effective.
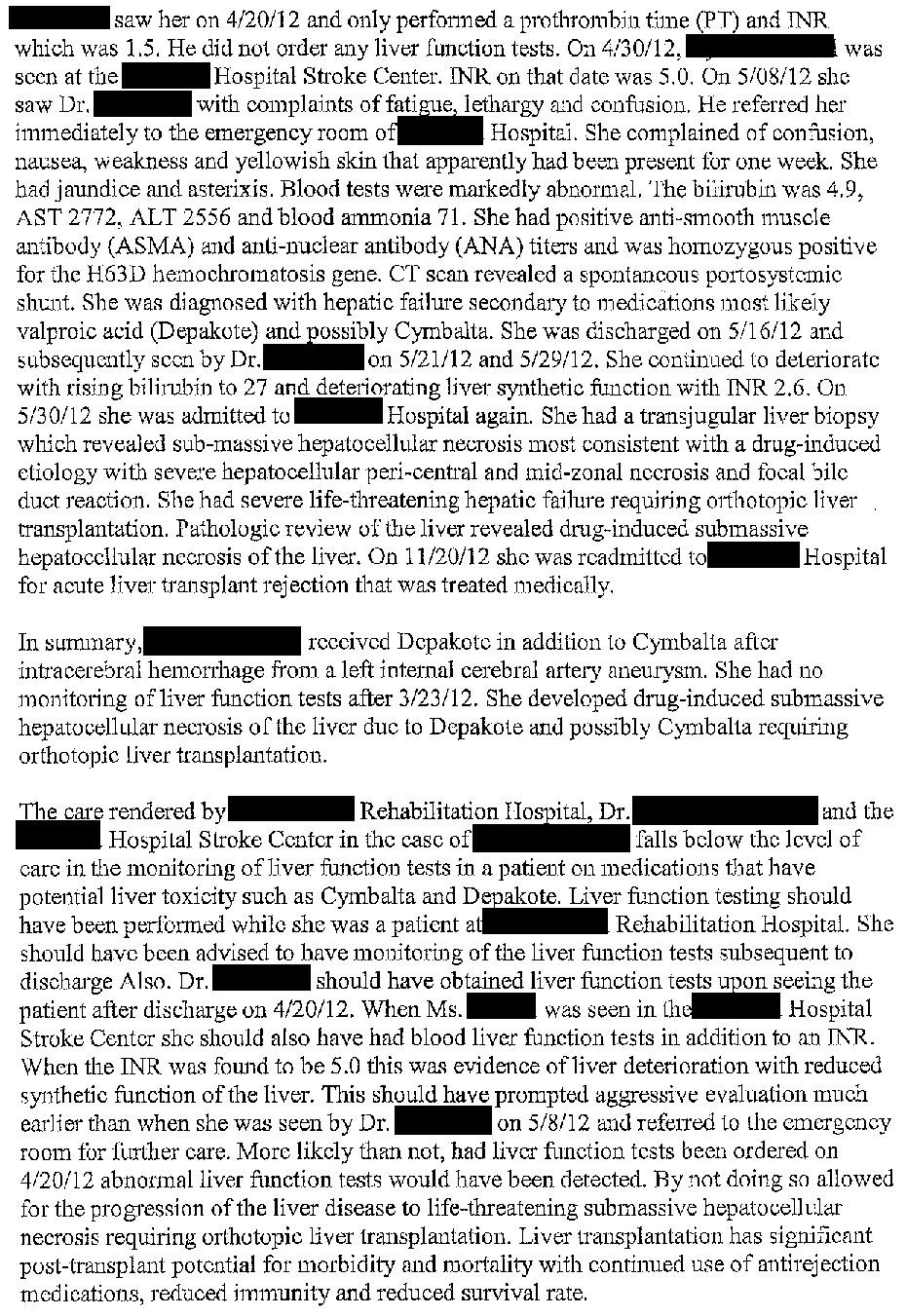
While she was in the hospital, she was started on Depakote. It was prescribed for both seizure prophylaxis and to treat agitation secondary to delirium.
Her AST, ALT, and bilirubin were all normal throughout her hospital stay, including on the day of discharge.
The Depakote was continued during her time in a rehab facility, and on discharge home.
Join thousands of doctors and attorneys on the email list.
Free to join, paid options available for those who want to learn more.
Following her release from the rehab facility, she had appointments with her PCP and the stroke clinic.
The APRN who saw her at the stroke clinic referred her to the neurosurgery clinic, explicitly to see if she needed to continue the Depakote. The patient’s INR was checked at this appointment and was 5.0. Her warfarin dose was adjusted.
Unfortunately, the next day she began to feel ill.
She developed lethargy, confusion, jaundice, and was found to be in liver failure on readmission to the hospital. She was diagnosed with valproate hepatotoxicity.
After briefly improving, she worsened again.
2 months after being started on Depakote, she received a liver transplant.
The patient filed a lawsuit against the hospital, the rehab facility, her PCP, and the stroke clinic APRN.
The expert witness opinion is shown here:
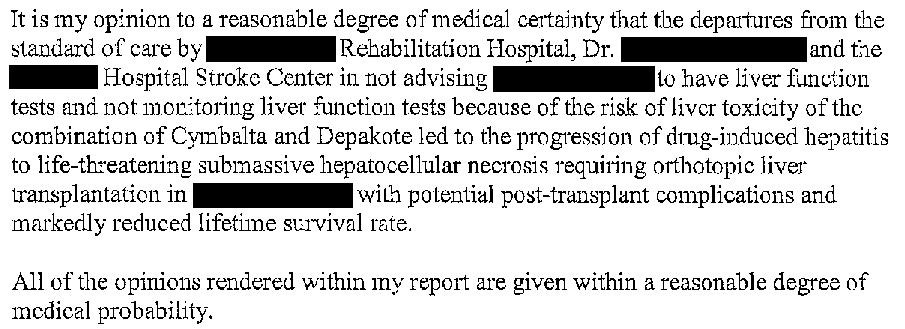
A second witness was also hired:
After extensive negotiations, a confidential settlement was reached.
Feedback from readers:
“If you are thinking about doing expert witness work, I would highly recommend paying for Med Mal Reviewer's subscription service. That site has tons of examples of expert witness testimony and it cites the fees charged by physician expert witnesses of various specialties. Generally a more experienced expert witness can command a higher fee.”
“I’ve personally learned a tremendous amount from these cases and want to give a big thank you.”
MedMalReviewer Analysis:
The expert suggests a combination of Cymbalta and Depakote as the cause of the patient’s liver failure. Depakote is by far the bigger suspect, especially considering that it carries an FDA black box warning for hepatotoxicity. Cymbalta does carry a slight risk of hepatoxicity as well, but it is not as clearly defined in the literature. I was unable to find any evidence for a synergistic effect from both medications together. If you are aware of any research to support this theory, please let me know in the comments!
She likely should have had the Depakote stopped when she was discharged from the hospital. It was started for seizure prophylaxis, but she never had a seizure and by the time she left the hospital, the risk of seizure was extremely low.
This case has a clear example of anchoring. The APRN at the stroke clinic knew the patient was on Coumadin and had an INR of 5.0. She made a (not entirely unreasonable) assumption that the patient simply needed a dose adjustment. She also knew that the patient was recently started on Depakote. The nurse practitioner failed to consider other causes of her elevated INR. This case is a good reminder to always expand your differential and to be wary of jumping to the most simple possible conclusion.
This malpractice case hinges on the theory that the doctors and NP were negligent because they did not recheck labs soon enough. The fact that the patient had a rare but well-known side effect from her medication does not warrant a lawsuit alone.
In this case, the time from starting Depakote to clinical symptoms of hepatotoxicity was about 5 weeks. Many guidelines suggest that repeat testing is not needed for 3-6 months after initiation, although this is primarily focused on using it for bipolar disorder. These guidelines give the defense a powerful counterargument.
Previous Cases:
Popliteal Artery Perforation [Subscribers Only]
Synopsis: Patient has acute popliteal occlusion, vascular surgeon does thrombectomy and atherectomy, causing popliteal artery perforation that is not discovered until the next day.
Synopsis: Patient has a kidney biopsy, Lovenox started several hours later. Patient has massive hemorrhage, started on pressors, which cause ischemia and amputation of 9 fingers.
Gentamicin Toxicity [Subscribers Only]
Synopsis: 18-year-old with Crohn’s disease has abscesses and a fistula. She is started on home gentamicin but a failure to monitor leads to ototoxic and nephrotoxic effects.






I wonder if the hemachromatosis contributed to the liver failure. Really interesting case!