A 35-year-old woman presented to her PCP with a right neck mass.
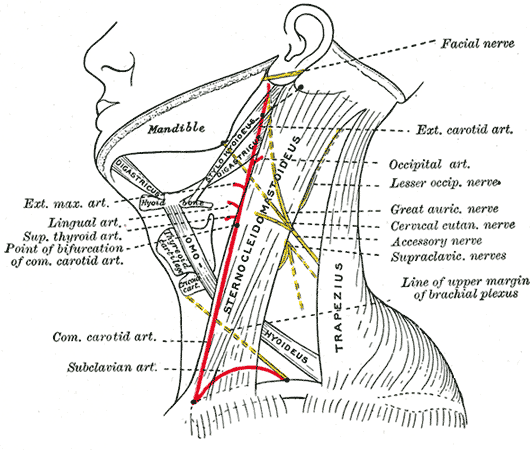
It was located on the posterolateral neck, between her sternocleidomastoid and trapezius.
She was HIV+ and took Truvada and Kaletra.
A referral was made to a general surgeon.
Workup was suggestive of an abnormal lymph node.
The general surgeon proposed excision of the neck mass.
A general surgery resident assisted with the operation.
The operative note is shown here, pulled from the expert’s opinion:
Over the next few days she noticed drainage and severe pain at the operation site.
An ED visit did not reveal any specific complications.
She had multiple follow-ups with the general surgery clinic.
She had neck pain and right shoulder pain that continued longer than expected.
After several months, an MRI of her cervical spine was ordered.
Following the MRI, she followed up with a neurologist.
The MRI did not show any abnormality of her cervical spine.
The neurologist did a full exam, and diagnosed an accessory nerve (CN XI) palsy.
She was given a referral to an orthopedist.
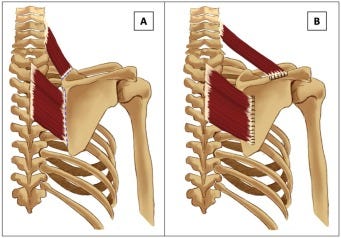
An Eden-Lange surgery was done to restore partial function. Nearby muscles with preserved innervation are repositioned to improve control of the scapula.
Join 10,000+ doctors and attorneys on the email list.
Free to join, paid upgrades for those who want weekly cases.
The patient hired a personal injury law firm.
They sued the attending surgeon, his medical group, and the hospital.
The expert witness opinion is shown here:
The plaintiffs have offered to settle for $750,000.
The lawsuit is ongoing.
Join the email list to be notified when there are new developments.
MedMalReviewer Analysis:
I really enjoy cases that connect basic topics (like anatomy) to real-world practice. One of the key learning pearls here is that the accessory nerve runs through the posterior triangle of the neck. Recall that the posterior triangle is bounded by the sternocleidomastoid, trapezius, and the clavicle.
The most common cause of CN XI injury is iatrogenic damage during neck surgery, especially lymph node biopsies. As a generalist, consideration of the exact anatomical course of the accessory nerve (CN XI) is not a part of my daily practice. Surgeons operating on the neck are intimately familiar with this issue, and need to keep a high degree of suspicion. I am surprised it took multiple months for this to be properly diagnosed.
Diagnosing a CN XI injury can be challenging if you’ve never seen one before. Most patients do NOT present reporting paralysis. The most common presenting symptom is shoulder pain. Some may describe it as neck pain or upper back pain. This is likely due to overcompensation by other muscles in the region and strain on the brachial plexus. Many patients also describe shoulder weakness with normal activities such as putting objects into a cabinet. (Source)
Another challenging issue is that the appropriate exam requires direct visualization of the patient’s neck, shoulder, scapula, and upper back. This is nearly impossible without removal of their shirt and undergarments, a step that is often skipped in fast-paced environments. Asymmetry of the shoulders and scapular winging are often present.
I recently started offering institutional subscriptions for residency programs.
Reply to this email or via admin@medmalreviewer.com for more information.
Facebook banned this newsletter, this is the only link that still works for sharing: https://substack.com/profile/9224497-med-mal-reviewer
I’d appreciate it if you shared it!







Thanks for an anatomical case. Also, I’m surprised at what appears to be a low settlement offer.
It’s amazing what expert witnesses will say to favor the plaintiff. They quote both the operative note and consent form that patient was consented to nerve injury as a known complication, yet conclude that SOC was deviated from. It’s unfortunate the patient is now left with this disability, but I doubt this stands a chance in court because of the good documentation.