A 58-year-old woman presented to the ED with burning chest pain that started 2-3 hours earlier while sitting on a porch swing.
Her first set of vitals were documented:
BP 116/57
Pulse 94bpm
Respiratory rate 24/min
O2 sat 90% on room air
Temp 97F
She had been cleaning a Jeep in the sun, and was sunburned.
Past medical history included Crohn’s disease, hyperlipidemia, hypothyroidism, and she smoked 1ppd.
Her EKG is shown here:
The automated EKG interpretation was “sinus rhythm with sinus arrhythmia, right atrial enlargement, rightward axis, possible anterior infarct, age undetermined, abnormal ECG”.
The physician documented “normal sinus rhythm”.
Join thousands of doctors on the email list.
The patient was given 0.4mg nitroglycerin SL, which did not change her pain.
She was given 500mL of normal saline and IV Toradol 30mg.
CBC and CMP were unremarkable.
A troponin was normal at 0.06 (normal range 0.00 - 0.10).
CK MB was 1.9 (normal range 0.0 - 3.6).
A chest x-ray was unremarkable.
The physician documented that she was “improved” and the patient was discharged.
The following morning, the patient collapsed in the kitchen in front of her family.
EMS arrived to a pulseless patient in V fib.
She was successfully defibrillated and taken back to the ED.
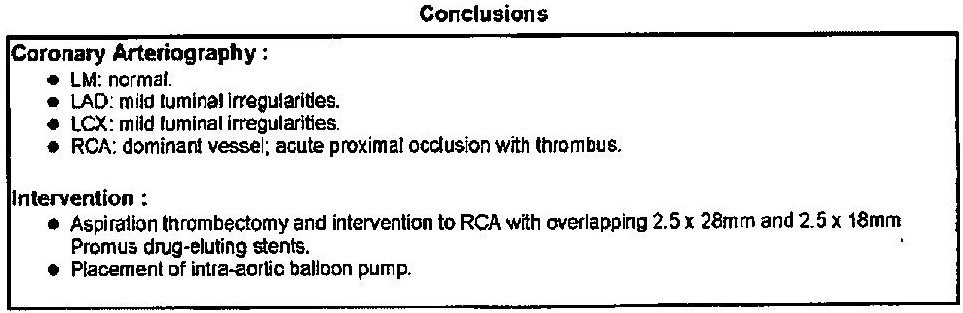
After being transferred to an academic center, she was taken to the cath lab:
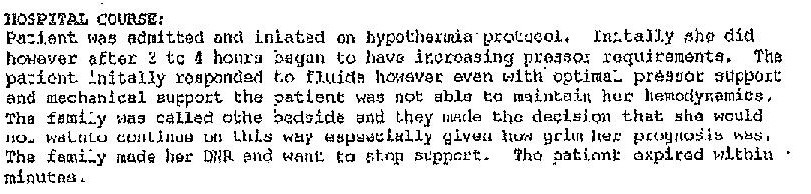
Unfortunately, she continued to decline despite aggressive measures.
The family elected to switch to comfort care and she died.
An excerpt from her death summary is shown here:
The family filed a lawsuit against the physician and the hospital.
They sued the the county-operated EMS service for allegedly not dispatching the call fast enough.
They also sued both EMTs for allegedly not starting chest compressions and defibrillating quickly enough.
The opinion from the defense EM expert is shown here:
Protect yourself.
Become a better doctor.
Paying subscribers get a new case every week and access to the entire archive.
The EMTs were found to have personal immunity as part of their employment with the local government. They were dismissed.
The 911 call center and EMS service were also dismissed.
The hospital and doctor reached confidential settlements.
MedMalReviewer Analysis:
After originally working on this case several years ago, I became interested in re-analyzing it in light of The OMI Manifesto. In short, the OMI paradigm offers an improved method of EKG interpretation that seeks to replace the STEMI/NSTEMI dichotomy that currently dictates emergency cath lab activation (but is rife with false positives and false negatives). While initially promising, I grew frustrated with the OMI model due to the extreme nuance it mandates in EKG interpretation, and my own inability to identify findings that the OMI experts claimed were obvious. I remain skeptical that the average physician should be expected to unilaterally interpret EKGs to the level of the OMI experts.
However, my frustration quickly reversed with the release of the Queen of Hearts algorithm, which was trained by Dr. Stephen Smith using AI to detect occlusion myocardial infarction that is often missed using standard STEMI criteria. It allows users to take a picture of an EKG, which is digitized and then analyzed for OMI.
Naturally, I ran the EKG from this case through the Queen of Hearts algorithm. Sure enough, it detected OMI with high probability:I was initially skeptical that the algorithm was just flagging everything as OMI. I repeatedly tested the algorithm with multiple other EKGs, and my anecdotal report is that I found it to be highly reliable.
This is the first medical AI product I’ve seen with the potential to actually improve the care we offer.
I see three distinct advantages:Help us catch subtle MIs that kill patients like the one in this case.
Avoid false positive cath lab activations (a source of constant argument between cardiology and the ED).
Use to triage new arrivals to the ED and avoid having to interrupt an ED doctor every 5 minutes to look at an EKG.
I’m sensitive to the fact that early promise doesn’t always play out in the long run, and that more research needs to be done. But I’ve seen enough to feel very hopeful.
Note: This is not sponsored in any way, no one involved with the Queen of Hearts is even aware that I’m publishing this.Nothing has changed faster in my 6 years as an attending EM physician than care of chest pain patients. When I was a resident, chest pain was the easiest chief complaint in the world. They all got hospitalized for chest pain observation (obviously, barring true emergency findings such as STEMI, PE, dissection, etc…). Now things have totally changed, and we’re sending the vast majority of chest pain patients home.
There’s a lot of hospital-to-hospital and doctor-to-doctor variation here, but from my perspective we’ve progressed through 3 Eras of Chest Pain Management:Admit everyone for a stress test
Discharge low HEART score, admit all others for a stress test
Discharge everyone (cards couldn’t care less if HEART score was 0 or 10), only admit if a patient has 2 high sensitivity troponins with a positive delta
This case happened in 2011, when most chest pain patients were getting admitted regardless of a negative workup. Given the rapid changes in chest pain management, its hard to mentally switch to the standard of care in 2011 (I bet a good portion of readers weren’t even practicing medicine then). The doctor didn’t have the benefit of high sensitivity troponins. He though the pain had been present for at least a few hours, so it didn’t seem necessary to do a repeat troponin. The symptoms were very atypical (started at rest, burning sensation, reproduced with palpation) and the sunburn provided a clear alternative explanation for burning pain. There are nonspecific EKG findings, but often times subtle depressions turn out to be nothing. Her chest pain seemed to improve. I can see good arguments either way on this case. Even if this patient had been admitted, the only thing that might have changed was an in-hospital cardiac arrest instead of an out-of-hospital cardiac arrest. Admission might have increased her odds of survival by a tiny bit but certainly was no guarantee.
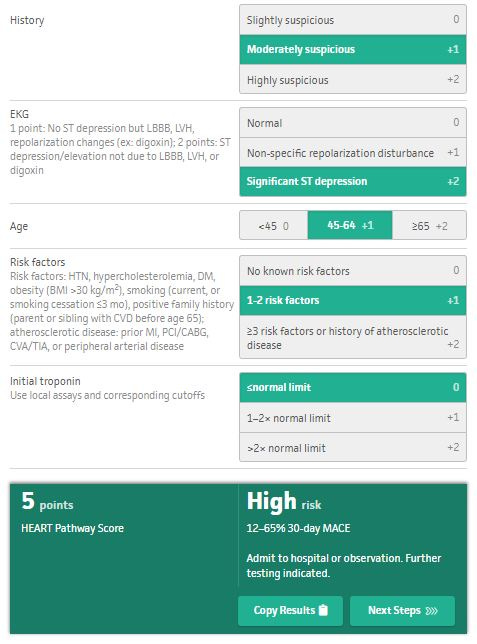
The HEART score didn’t come out until years after this case, but its worth considering for learning purposes. I calculate it to be 5. This is a high risk HEART score, and could be used to push for admission.
I give the patient 2 points for EKG in light of the ST depression in V4-V6. There are some other potential EKG findings but the morphology is odd. There is a wandering baseline in I and each heart beat has a different morphology in aVL which makes it hard to draw any conclusions. The ST elevation in aVR ranges from 0mm to 1.75mm depending on which heart beat you look at. One universal lesson from this case is if you have an odd-looking EKG or are unsure, get a repeat EKG. I’m looking forward to all the comments from the self-appointed EKG experts!

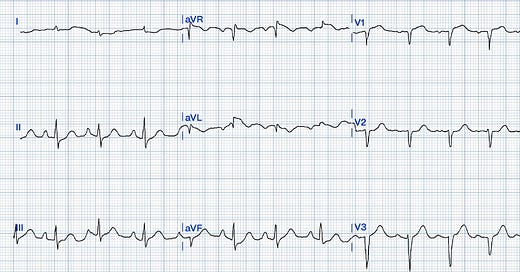


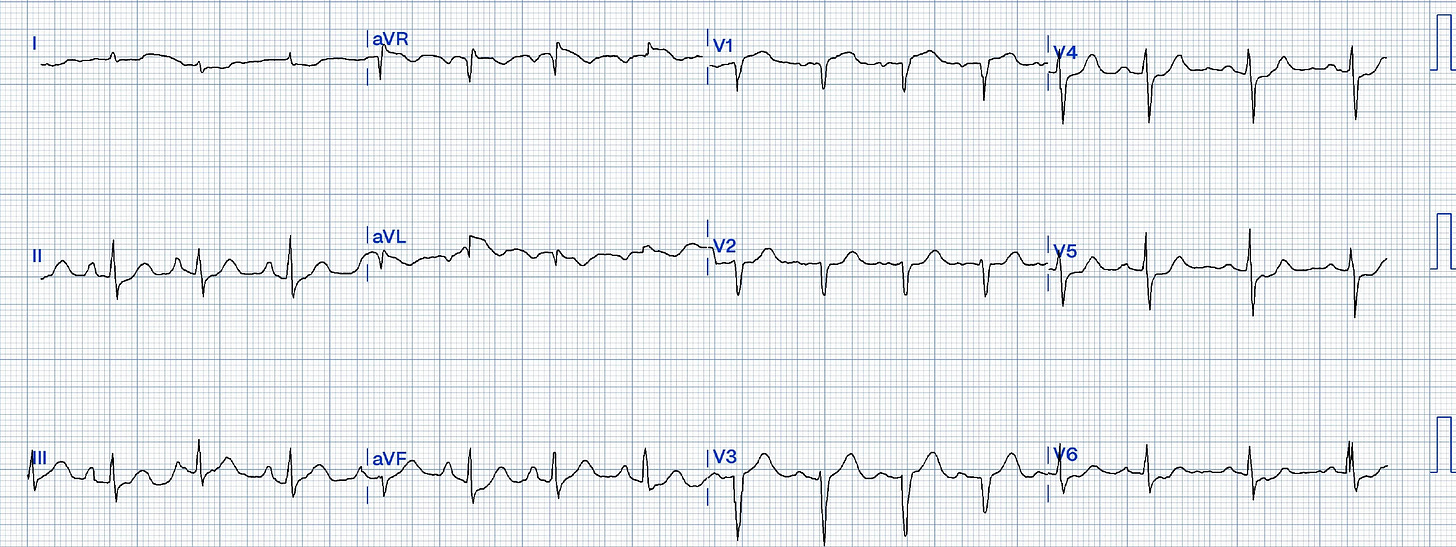







I don’t claim to be an EKG expert, but this EKG is pretty clearly abnormal and warrants at the very least a repeat EKG or comparison with previous. additionally, even in 2011, a single troponin of the low sensitive variety would not have been standard of care for discharge from the ED.
Gotta say, even in 2011 this reads as a miss. I finished EM residency in 2011 and at that time a single troponin in someone with chest pain after “2-3 hours” would not have been standard of care. It was pretty well accepted at that time that it takes at least 3-5 hours for a troponin to be detectable on laboratory evaluation after the onset of pain. Additionally, while a troponin value of 0.06 was within the reference range, unless you had a baseline troponin (in the 2011 era) most people considered that value a gray zone. All of this is to say a second troponin would have been standard of care in this case. A single troponin was being done in a performative manner as a way to quickly discharge the patient and not actually to evaluate chest pain. That is the miss.
There are many aspects of this case that read as a miss but I want to echo that this EKG was simply misread. It is not normal in any way. There are easily seen depressions in V4-6 as well as lead I (admittedly a bad baseline but still the ST segment is not normal). Unless there is a baseline EKG for reference that show those changes as baseline you either need to repeat the EKG to confirm those morphologies or assume those are new findings.
For me reading this case, it appears the physician thought this was BS chest pain and in turn did a BS work up just to assuage the patient of his assumption. We all do this from time to time and this physician lost that gamble this time. Even in 2011 this was a miss