A 62-year-old man was seen by an orthopedic surgeon for pain in his shoulders.
A shoulder arthroscopy was recommended.
The orthopedist ordered pre-op labs and an EKG.
The patient was referred to his PCP for a pre-op evaluation.
His PCP practiced both primary care and gastroenterology (he had completed an IM residency and GI fellowship).
He had been taking care of the patient for several years.
The patient’s medical history included HTN, hyperlipidemia, and obesity.
3 years earlier, he had failed a stress test. The subsequent cardiac catheterization revealed non-obstructive coronary artery disease.
5 days after the labs and EKG, he saw his PCP and was authorized to undergo surgery.
He did not feel any repeat cardiac testing was needed.
His PCP did not know that an EKG had been done.
Per court records, the automated EKG interpretation noted ST elevations.
Unfortunately for us, the lawyers did not file this EKG in the public court records.
However, we do know he was not having any chest pain, shortness of breath, or any symptoms that could be considered anginal equivalents at that time.
The surgery happened 28 days later.
The operation itself was uneventful and he was discharged home.
The next day, the patient collapsed at home without any warning.
His wife called 911.
He was rushed to the ED in cardiac arrest.
They initially achieved ROSC but he died 2 days later in the hospital.
An autopsy was done.
It showed multiple 70-90% coronary artery lesions and the final cause of death was acute MI.
Join 8400+ doctors and lawyers on the email list.
Subscribe today.
His family contacted an attorney and a lawsuit was filed.
The physician and his employer were named as defendants.
The patient’s estate offered to settle the lawsuit for $1,750,000.
His wife offered to settle for $250,000.
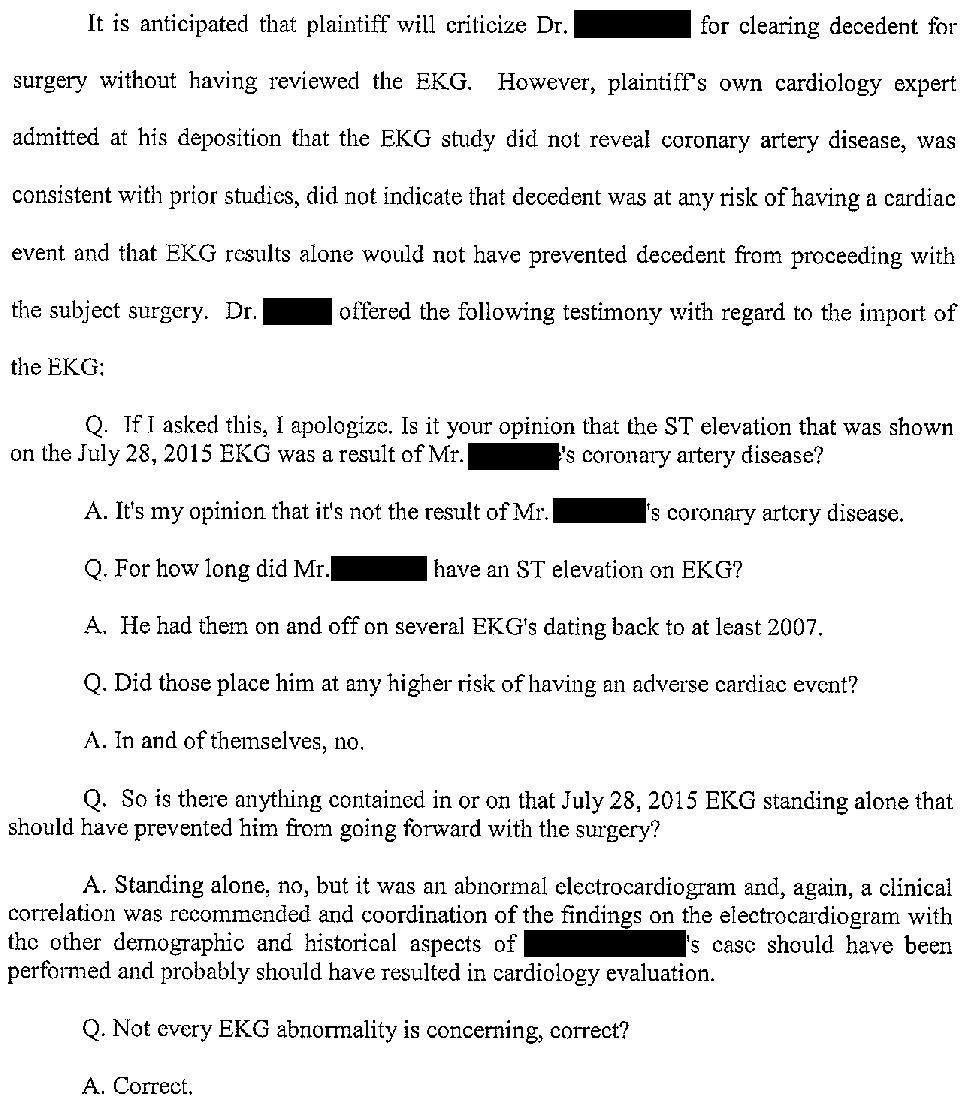
The plaintiff’s cardiology expert was deposed.
He suggests that the surgery caused SIRS (independent of any infection), which in turned caused the cardiac arrest.
The defense noted that none of the literature supports the idea that surgery would cause SIRS, and in turn cause cardiac arrest.
The doctor’s defense attorney filed a motion seeking to ban the plaintiff from mentioning the EKG at trial.
Usually the plaintiff would have the opportunity to file their response to this motion, and then judge would issue a decision about allowing this information at trial.
However, prior to this the two sides reached a confidential settlement and the lawsuit was withdrawn.
Become a medicolegal expert. Read a new case every week.
Pick up a subscription today.
MedMalReviewer Analysis:
The deposition testimony from the cardiology expert witness is quite bizarre. Talking about SIRS would make sense in the context of an infection or sepsis, but this case has nothing to do with that. It seems like he got flustered when asked about the exact mechanism of operative cardiac stress. He tried to make his argument seem more valid by referencing the first official-sounding syndrome he could think of that contained the word “inflammation”, rather than the general concept of inflammation.
This is the first time I’ve seen a defense attorney reference the scientific literature, which needs to be done more often.
This case is far outside my arena of medical expertise so I’ll leave the primary care doctors and cardiologists to comment on the necessary pre-op workup for a patient who last had a cath 3 years earlier showing nonobstructive disease.






Another frustrating case that illustrates the farce that is our medicolegal system. Many patients have baseline abnormal EKGs. The EKG being abnormal would not have stopped the surgery from proceeding if it was like that at baseline. Furthermore, if the patient did not have clinical anginal equivalents and had reasonable baseline performance status (greater or equal to 4 mets) then no pre-operative risk stratification would have been recommended - regardless of if the person doing the eval was an internist or a cardiologist. The standard of care would have been met. The problem is that shit happens. And shit can happen more if you are older with multiple cardiovascular risk factors. But by over-testing, you are exposing the patient to the risks of testing without necessarily making their operative risk lower. You could easily find a lesion, cath the patient, never have made a difference in their perioperative outcome, but put them at risk of a cath related adverse event like a hematoma or CIN. You can't work backwards from "something bad happened" to "something must have been missed" because in reality, shit happens. What would help the internist would be a well reasoned pre op note and ideally use of an evidence based risk calculator like NSQIP.
As for the cardiologist's opinion, I am honestly embarrassed for them. What are they even talking about? It's true that cutting into tissue can cause inflammation and certainly noninfectious systemic stress can cause SIRS. But SIRS is at least in part defined by abnormal vital signs, in contrary to what the cardiologist said. Post-op systemic inflammatory stress can certainly cause plenty of issues and likely contributes to delirium, sometimes low grade fevers, sometimes low grade leukocytosis, a-fib, other cardiovascular events, and other complications. And regardless of how SIRS is defined, it has absolutely nothing to do with the issue at hand, which is the pre-op eval. We aren't trying to prevent inflammation with the pre-op eval - that makes no sense as a goal. Systemic inflammation can certainly cause a coronary plaque to rupture but then the question goes back to: is finding and fixing every plaque considered the standard of care? Of course not. We know that fixing asymptomatic lesions does not improve outcomes generally. If the patient had good performance status and no active anginal symptoms (as well as an EKG unchanged from baseline), then finding and fixing lesions would not have been the standard of care and in fact may come across as unscrupulous. What happened to this man falls into the "shit happens" category. Shit happens to everyone. If shit didn't happen, we'd all live forever.
I hate our medical system. What is wrong with us?
-an annoyed hospitalist
In my preop note template I like this phrase in which I took from a cardiologist. I try to document like a porkypine.
"Per ACC/AHA peri-operative guidelines, moderate risk surgery and METS >=4 is low risk for MACE and no further cardiac testing is required. Pt has no active cardiac condition (ACS/USA, decompensated CHF, ventricular arrhythmias or severe valvular disease) and can easily achieve > 4 METS. Pt does not require further cardiac evaluation prior to undergoing surgical procedure. These recommendations follow the 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. (JACC Vol. 64 No. 22, Dec 9, 2014, pp e77-e137).
Evaluating Risk in Surgery is a combination of patient’s risk factors and surgical risk factors. Patient is being evaluated for medical optimization and not “surgical clearance”. MACE is the major adverse cardiovascular event risk, and can be assessed based on the Revised Cardiac Risk Index score."
I also include the RCRI score in my note
RCRI = rate of major cardiac event
Six independent predictors of major cardiac complications:
(-) High-risk type of surgery (examples include vascular surgery and any open intraperitoneal or intrathoracic procedures)
(-) History of ischemic heart disease
(-) History of HF
(-) History of cerebrovascular disease
(-) Diabetes mellitus requiring treatment with insulin
(-) Preoperative serum creatinine >2.0 mg/dL (177 micromol/L)
Rate of cardiac death, nonfatal myocardial infarction, and nonfatal cardiac arrest according to the number of predictors:
0 = 0.4 percent (95% CI: 0.1-0.8)
1 = 0.9 percent (95% CI: 0.5-1.4)
2 = 6.6 percent (95% CI: 1.3-3.5) .
3+ = 11 percent (95% CI: 2.8-7.9)