A 57-year-old woman presented to the ED on January 6 with lower abdominal pain.
Workup included CT scan and labs.
Results did not show any emergency findings.
The CT suggested “abnormal densities in the pancreatic head”.
She was prescribed Zofran, referred to GI, and discharged.
Over the next 3 weeks her abdomen continued to hurt.
She was taking 10 aspirin each day as well as Vicodin from a prior prescription.
She returned to the same ED on January 30 (26 days after her first visit).
The ED physician ordered labs and IM ketorolac.
He reviewed the prior CT and did not feel that a repeat was necessary.
Nurse notes indicate she was “screaming in pain” 15 minutes before discharge, but the physician’s note indicates that she had resolution of her pain.
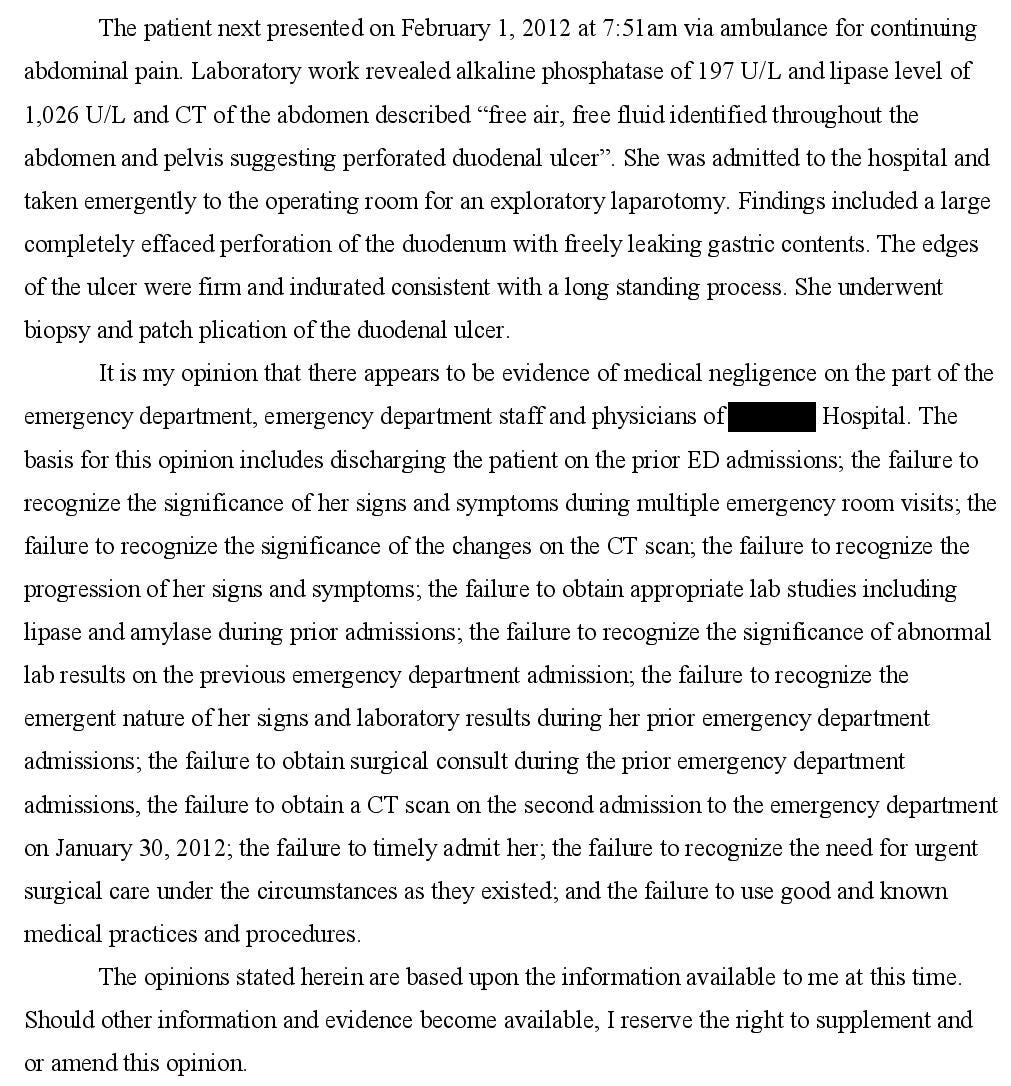
2 days later she returned again with abdominal pain.
CT showed free air, from a duodenal ulcer perforation.
She survived but had a long and difficult recovery.
Join 7000+ doctors and attorneys on the email list.
Subscribe today to get a new case every week.
She hired an attorney and sued the doctor from the 2nd visit.
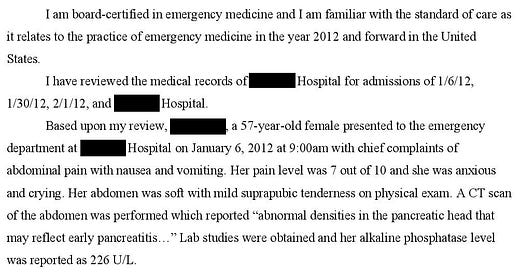
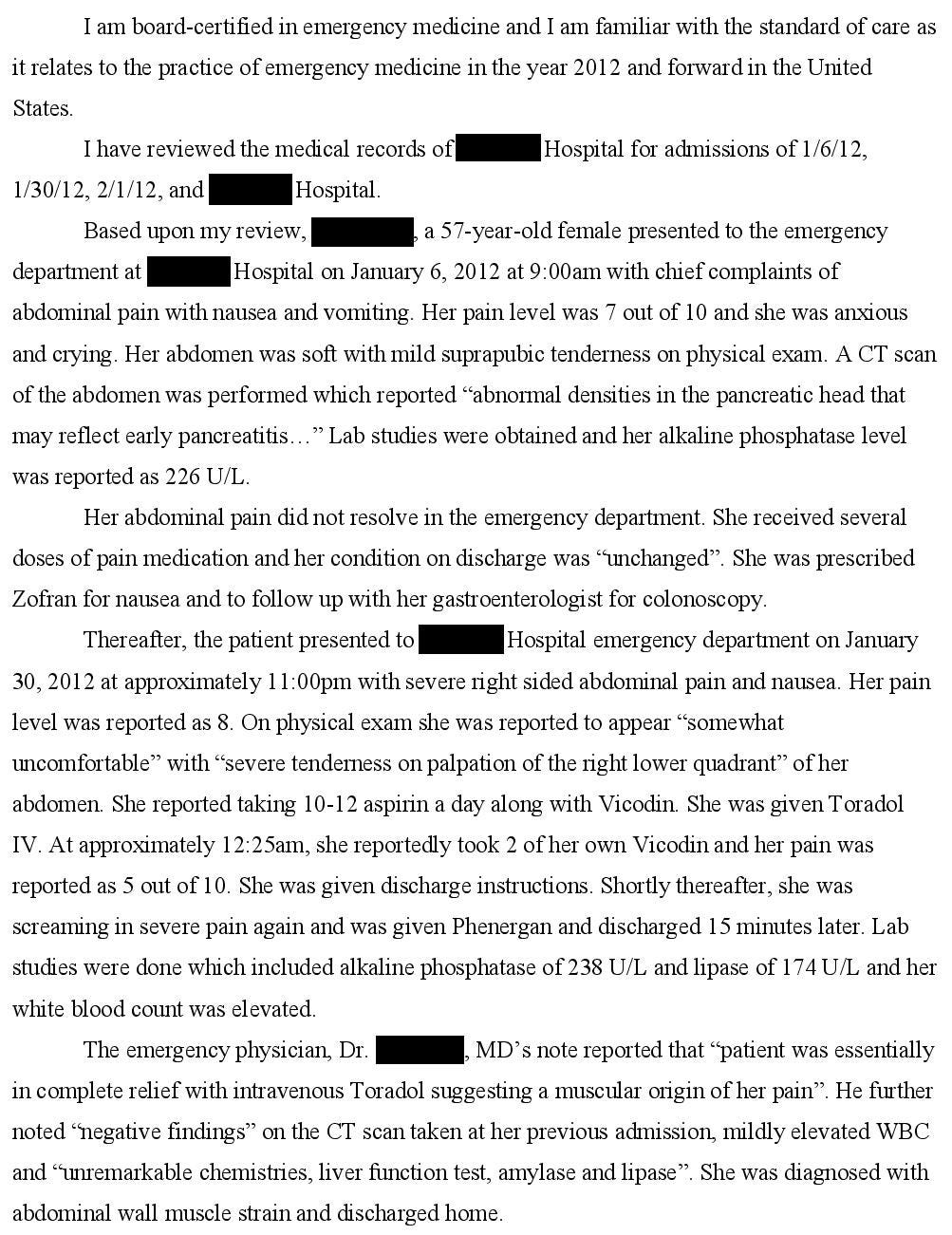
The plaintiff’s expert witness opinion is shown below:
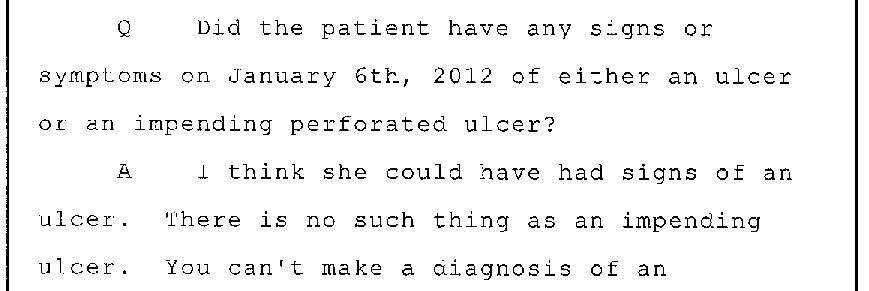
The defense attorney deposed the plaintiff’s expert witness:
The lawsuit was settled for an undisclosed amount.
MedMalReviewer Analysis:
EM physicians are often ridiculed for ordering too many CT scans. Unfortunately, this doctor was sued for the exact opposite issue.
The excessive use of aspirin was the clear red flag in this case. The initial visit for abdominal pain may have had nothing to do with the duodenal ulcer that caused the perforation. Adding a dose of ketorolac on top of this certainly did not help.
Additionally, it would have been wise to check a salicylate level.Pain that improves after ketorolac does not necessarily indicate a musculoskeletal etiology. The doctor diagnosed her with an abdominal wall muscle strain, which was clearly incorrect. Unless you are absolutely sure about the diagnosis, it is better to simply make the final diagnosis the same as the chief complaint. If the patient has a bad outcome, it is preferable to have a vague but not incorrect diagnosis, rather than a specific and wrong diagnosis.
This is a classic example of older patients with abdominal catastrophes presenting with pain in the “wrong” location. She had a perforated duodenum with pain in the RLQ, not the epigastrium. The older the patient, the less you can trust a differential that is built based on the location of their pain.
Reader Feedback:
“If you want to learn how to write expert reports, the MedMalReviewer service is really good. I read it all the time….
I'm a lawyer who routinely hires expert witnesses (in non medical fields). Some pieces of advice: always talk to the lawyer hiring you on the phone. No emails. You'll need to have every communication you make about the case available to turn over to the opposing attorney. It's much easier if you haven't sent many, or any, emails.”
Previous Cases:
Lethal Rash [Subscribers Only]
Patient started on new medication and goes to the ED after slowly developing a rash. Admitted to the burn center, where medication is accidentally re-started, and she dies.
Diabetic patient given dextrose, develops compartment syndrome of the forearm.
Prisoner Meningitis [Subscribers Only]
25-year-old in jail develops fever, headache, vomiting, tachycardia. Requests for medical attention largely ignored, patient dies.



The more I read these cases, the more I realize that I can't help but be biased toward the defendants. I can imagine what was going through the ED attending's mind.
I wonder if simple documentation stating that the patient was told to avoid aspirin, take a PPI and follow up with GI would have been enough to save this attending from a lawsuit, regardless of whether or not the duodenum perforates.
I'm a pharmacist and this case is making me pull my hair out!