Editor’s notes:
Thanks to Dr. Kurt Lucas for sending me this case! If you know about a malpractice lawsuit I should cover, send it to me by replying to this email.
As a reminder, it is my long-standing editorial policy to always censor out patient and doctor names, even when a quick Google search might reveal this information. My goal is to share medical and legal learning points, not operate a “name and shame” tabloid.
A 13-year-old girl was bitten on her foot by a rattlesnake at around 8:20pm.
Her father killed it, took a picture, and called 911.
They brought the dead snake to the ED as well.
This is the actual picture of the snake from the scene:
The patient was seen by the ER doctor at 9:20pm.
This is how her foot looked shortly after arrival to the ED:
A CBC, BMP, and coag panel were ordered.
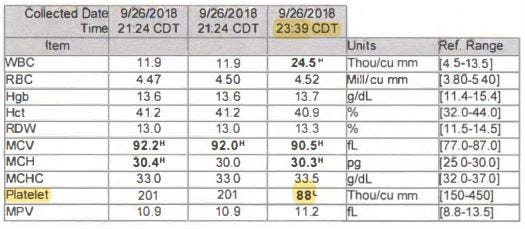
The initial labs and a repeat blood draw are shown below. The BMP was normal.
The doctor and nurses initiated the hospital’s snakebite protocol.
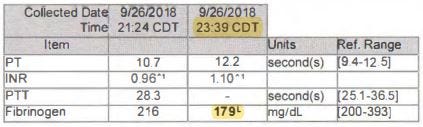
They filled out a Snakebite Severity Score (SSS).
She was initially given a 2, then revised upward to a 3 several minutes later due to development of paresthesias in the toes.
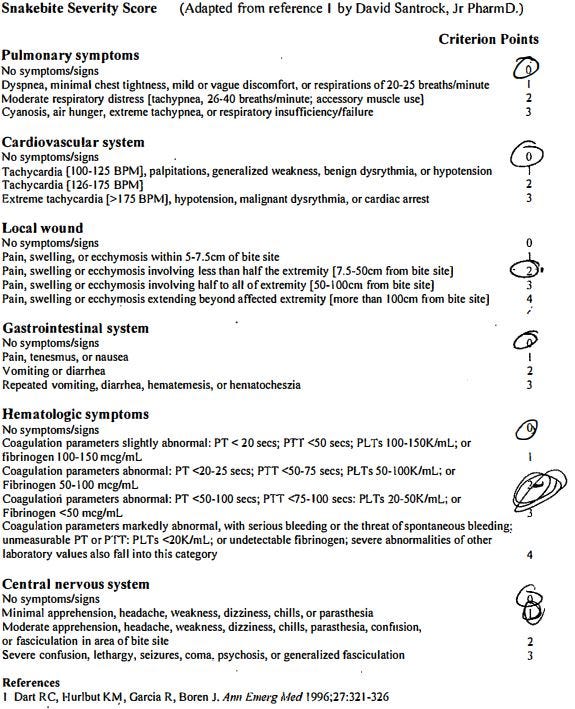
They decided not to give Crofab based on the protocol’s decision tree.
The patient’s pain began to creep up her leg.
The areas of pain were marked at different times during the nurse’s reassessments.
Repeat labs were drawn at 23:39, showing decreased fibrinogen and thrombocytopenia.
Her Snakebite Severity Score had risen to a 5.
The doctor ordered Crofab at 23:50 and the infusion was done by 00:29.
The patient was transferred to a pediatric medical center.
At the receiving hospital, the redness and swelling significantly worsened.
She was given additional Crofab.
After several days, the appearance of her leg was improving.
She worked with physical therapy and was discharged with crutches.
The patient and her family report permanent pain and dysfunction in her leg.
Join thousands of doctors and attorneys on the email list.
The patient’s family was very upset about her lingering symptoms.
They blamed the doctor for not giving Crofab immediately upon arrival.
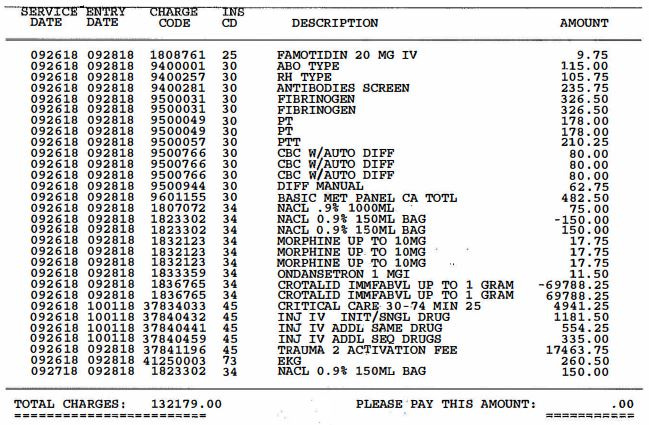
The hospital agreed to write off the entire bill.
An excerpt from the itemized bill is shown here:
Note the Crofab fee of $69,788.25 and a level 2 trauma activation fee of $17,463.75.
Nonetheless, a lawsuit was filed against the ER doctor.
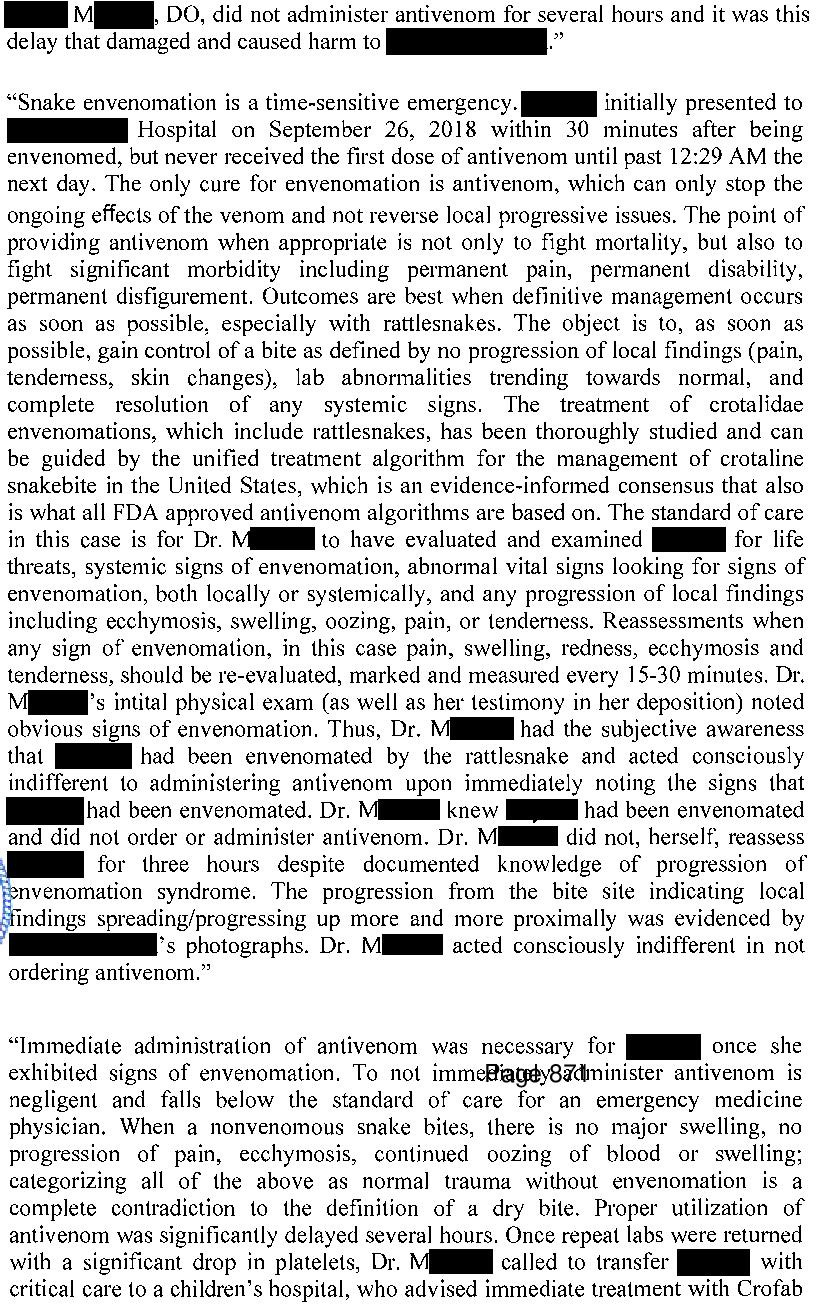
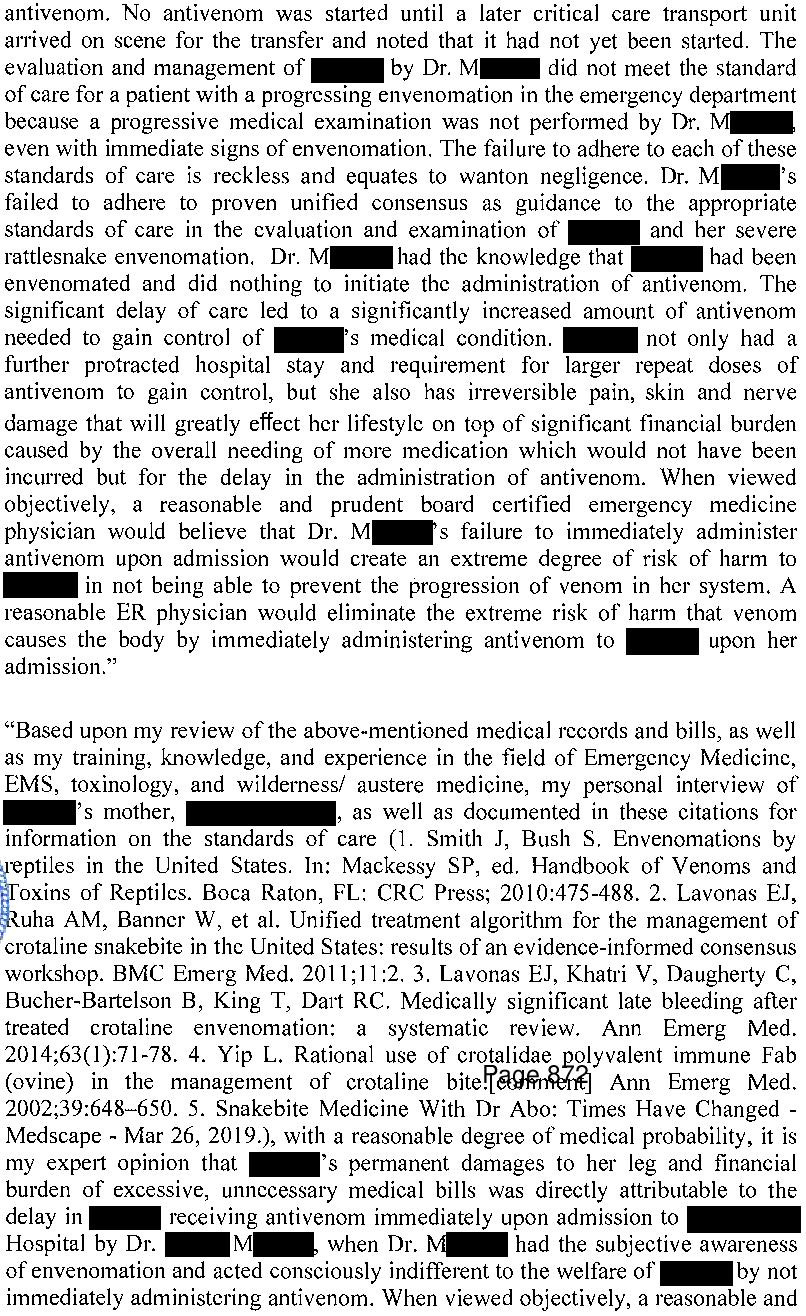
An out-of-state EM physician was hired to write an expert opinion.
The state in which this happened has a law that requires plaintiffs to demonstrate that the defendants acted with “willful and wanton” negligence if the case involves emergency care.
The judge felt the doctor’s actions did not rise to this level, and dismissed the lawsuit.
The plaintiffs appealed.
They argued that only a physician can practice medicine, not a hospital protocol.
In their eyes, the doctor displayed gross negligence by not immediately giving Crofab, even if the hospital protocol said otherwise.
The appeals court reversed the initial judge’s decision:
Paying subscribers get a new case every week.
Subscribe today to expand your medicolegal expertise and improve your practice.
The defense then appealed to the state’s Supreme Court.
The Supreme Court reversed the appeals courts’ decision and reinstated the trial court’s dismissal of the lawsuit.
MedMalReviewer Analysis:
I agree with the Supreme Court that the doctor did not display willful or wanton negligence. Crofab is not a risk-free medication, and it is extremely unwise to advocate instantly ordering it for any relevant envenomation. The package insert for Crofab notes hypotension and angioedema as possible risks. The thoughtful approach the doctor displayed by following the algorithm is the correct way to balance the risks and benefits involved with both the snakebite itself and the administration of Crofab.
I find the expert’s opinion somewhat disturbing at several points.
It is littered with state-specific legal buzzwords that make it clear that it was heavily coached by the plaintiff’s attorney. A physician’s opinion should stick to the medical facts and experts should not allow attorneys to inject their own parasitic language that perverts the doctor’s sober analysis.
The expert states that he called and spoke with the patient’s mother. This is very bizarre. I’ve reviewed thousands of lawsuits, and I’ve never seen an expert mention that they personally called a patient or family member. An expert might review a deposition of a family member, or an independent medical exam (IME) might be conducted by a doctor, but most experts don’t call the plaintiffs and conduct their own homemade deposition. This is an obvious source of bias, especially in light of the fact that he never called the defending doctor to get her side of the story.
ACEP’s lawyers filed an amicus curiae brief with the Supreme Court on behalf of the doctor. This was an important piece of advocacy given that this case threatened to erode the “willful and wanton” / gross negligence standard in this state. Many EM physicians have mixed feelings about ACEP, but I would be remiss to not point out the importance of their advocacy for this individual physician and the specialty as a whole.
Editor’s update, February 12, 2024:
I was initially critical of the expert’s claims that the unified treatment algorithm was the only definitive standard, when other scores exist including the SSS.
However, I got feedback from several toxicologists, advising that using the Snakebite Severity Score (SSS) to guide the decision to give Crofab was not ideal.
The SSS was developed for research purposes, not to guide clinical care.
In fact, the lead author of the SSS (Dr. Richard Dart) wrote a letter in 1996 saying that it was not meant to guide treatment of individual patients, and that further research should be done to validate it for clinical use.
Most of the toxicologists I got feedback from suggested that they would give Crofab immediately for any rattlesnake bite that shows any sign of true envenomation.
Agkistrodon species (water mocassins, cotton mouth) bites are often less severe than rattlesnake bites, and it seems that some experts might be more inclined to use an algorithm (Unified treatment algorithm, not SSS) to guide decision-making, although there is debate about this.
The toxicologists also point out that the doctor could have called poison control to get expert advice, as opposed to relying on the questionable hospital protocol that led to delayed Crofab administration.









This poll tells me that 6% of you need to be stripped of your license to practice medicine. A freaking trial judge has more common sense than all of you. Gross negligence my a**. The other 19% need to review snakebite guidelines or stick to your lane (if not EM or Tox).
I re-read this case as we move into warm weather and walk into snake territory. This time I read the link to Dr. Dart's reply in your addendum. Dr. Dart, in 1996, wrote this pearl of wisdom: "Inadvertent, even if well-meaning, misuse of diagnostic tests is common in clinical medicine." 28 years later, we still run into the problem of research inclusion criteria and diagnostic definitions conflated as real-time clinical tools.