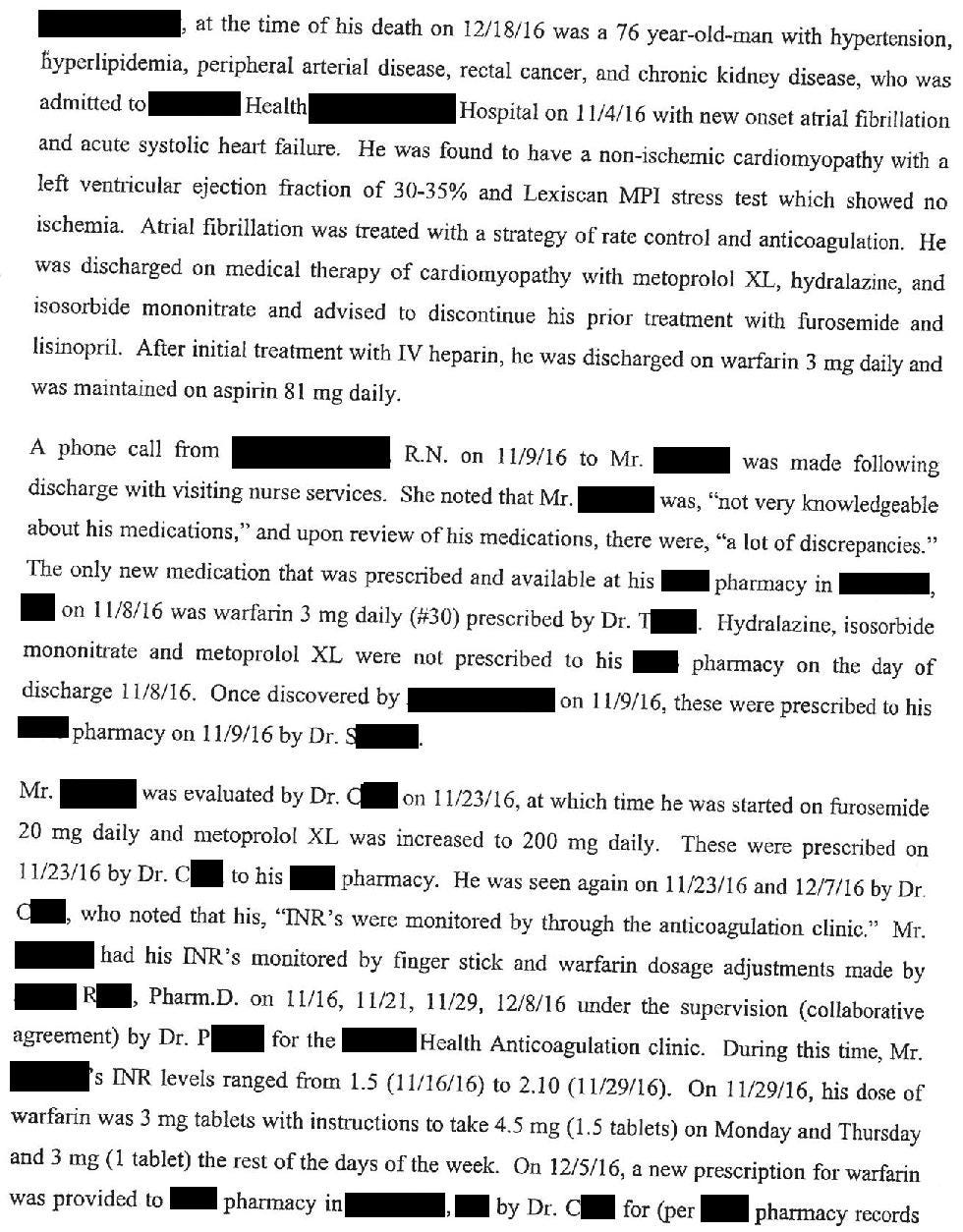
A 76-year-old man presented to the ED with new onset atrial fibrillation.
He was started on rate control and spontaneously converted back to sinus.
The patient was started on warfarin.
Dr. T (discharging hospitalist) wrote a prescription for warfarin 3mg qday, 30 tablets, no refills.
He was discharged on November 8.
Join thousands of doctors and attorneys on the email list.
Free and paid options available.
On November 16, he followed-up with the coagulation clinic.
His INR was 1.5, and he was continued on the same warfarin dose (3mg qday).
On November 23, he saw his cardiologist, Dr. C, who noted that the coagulation clinic was managing his warfarin.
He was seen again at the coagulation clinic on November 29.
His INR was 2.1.
He was instructed to increase the dose of warfarin to 1.5 tablets (4.5mg) 2 days per week, and one tablet (3mg) on the other days of the week.
The patient was running out of warfarin tablets, so he called Dr. C’s office for a refill.
The nurse called in a refill for his warfarin on December 5.
The message indicated that he should take “4.5” on 2 days per week, and “3” on the remaining days.
Unfortunately, the message was left without specifying the units of these doses.
The nurse meant 3 milligrams per day, but the pharmacist filled it as 3 tablets per day.
On the other days of the week, the prescription indicated he should take 4.5 tablets per day (as opposed to the correct dose of 4.5mg).
The patient followed up several more times with both Dr. C and the coagulation clinic.
No one realized the mistake until December 16, when his INR was checked at the coagulation clinic.
His INR was >8, higher than the point-of-care machine could read.
The patient had noticed increased bruising.
The pharmacist told the patient to hold warfarin and go to the ED if he started bleeding.
He was released to go back home.
An INR was sent to the lab, and that afternoon came back at 14.
The pharmacist notified the coagulation clinic’s supervising physician (Dr. P) by email.
The physician asked Dr. C’s office to send a vitamin K prescription to the pharmacy.
2 days later the patient was found in a massive pool of blood, having suffered a catastrophic GI bleed.
He died the following day in the hospital.
The vitamin K prescription was finally called into the pharmacy the same day he was found in a pool of blood at home.
The patient’s family sued the hospital, Dr. C (her cardiologist), Dr. P (supervised the coagulation clinic), and the pharmacy where the warfarin was dispensed.
The plaintiff’s expert witness opinion is shown here:
The lawsuit was bifurcated into 2 separate cases.
The case against the hospital and physicians remained in state court.
The case against the pharmacy (a large national corporation) was removed to federal court.
A settlement was reached with the pharmacy.
Most settlements are kept confidential, but due to a unique legal situation the settlement amount was disclosed in the court documents:
In state court, both doctors were dropped from the case.
This left the hospital as the only defendant.
Following an offer of compromise, a confidential settlement was reached.
Became a medicolegal expert.
Subscribe today to get a new case every week.
MedMalReviewer Analysis:
This case is fundamentally about a failure to communicate. The nurse and the pharmacist both felt that the instructions were clear, and didn’t realize the mistake until it was too late. Providing a written or electronic prescription would have reduced the likelihood of this error.
While I was reflecting on this case, I remembered the words of some of my math and science teachers from as far back as grade school, admonishing students to label their units. It can be frustrating for students to miss points because they had the correct number but didn’t appropriately label the units, but this case is a perfect example of why its important.
Medications with complicated dosing regimens are inherently more dangerous. This is readily apparent when comparing warfarin and factor Xa inhibitors. This case happened in 2016, long after the factor Xa inhibitors were available. I wonder if the higher price of the factor Xa inhibitors is what prompted them to choose warfarin.
The communication between the coagulation clinic and Dr. C’s office made this situation much worse. It appears that the coagulation clinic was responsible for monitoring his INR and suggesting changes, but they did not actually manage the warfarin prescription. The prescriptions were routed through Dr. C’s office, creating a game of telephone that introduced both errors and significant delays.
Anticoagulation-related malpractice lawsuits are unfortunately very common.
Here are a few I’ve published previously:
Vascular surgeon orders heparin drip for ischemic leg, patient’s INR was already 5.6, patient dies of head bleed. [Paid subscribers only]
Patient with a fib requests to stop taking warfarin, suffers massive stroke. [Paid subscribers only]
Warfarin bridge causes spinal hematoma and cauda equina syndrome







Hematologist here. Sad and unfortunate situation of miscommunication. As most of my patients who are treated with warfarin are elderly or comorbid with multiple medications I generally prescribe only one strength tablet (ie 5 mg tabs) and instruct the patient to take “by the tab”. For example 1 tab daily on weekdays and half tabs on weekends. I find prescribing in mgs for a drug that requires frequent adjustments to be too confusing for patients. Make sure your pharmacy and hospital are on board with this.
Why was the Coumadin dose decreased when the INR was 2.1? I know INR targets for a.fib to be 2-3 (non-valvular) or 2.5-3.5 (valvular).