A man in his 60s was seen for atrial fibrillation.
He had been on various medications for his arrhythmia, which had proven difficult to manage.
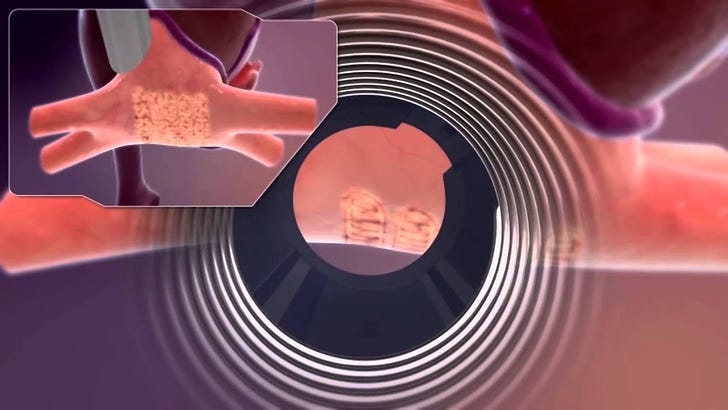
A hybrid maze procedure was recommended.
His anesthesia was managed by an anesthesiologist and a CRNA in the EP lab.
The patient suffered a respiratory arrest before the procedure began.
He was initially in PEA, but the anesthesia team quickly got ROSC.
Unfortunately he developed cardiogenic shock.
The patient was transferred to a large academic medical center.
He was placed on ECMO and a balloon pump.
He continued to decline and developed multi-organ failure.
He died 2 days after the initial respiratory arrest.
Join 7000+ doctors getting the best malpractice cases delivered to their inbox.
His wife hired an attorney and filed a lawsuit against the hospital and the anesthesiologist’ medical group.
Note that the anesthesiologist herself was not named as a defendant.
The specific allegations from the complaint are shown here:
The plaintiff’s expert witness opinion is shown here:
The law firm hired a financial expert (PhD in Economics) to assess the patient’s lost earnings.
The plaintiff offered to settle with the hospital for $2,500,000 and with the anesthesiologist’s medical group for $2,500,000.
The lawsuit reached a confidential settlement.
Become a medicolegal expert.
Subscribe to get a new lawsuit every week.
MedMalReviewer Analysis:
It is interesting that the anesthesiologist was not named as a defendant in the lawsuit. The plaintiff clearly is hoping for a multi-million dollar settlement, far above the typical limits on a physician’s malpractice insurance. These larger sums are typically only possible when suing a business such as a hospital, rather than an individual person.
We have a vague indication that a CRNA was involved in the patient’s care, but the lawyer did not include any details about their participation. The plaintiff displays no interest in their role, likely because there is little possibility for financial gain.
This case provides a good opportunity to review the hybrid maze procedure. While most doctors do not need to understand all the nuances related to it, reviewing the video above helps build a strong foundation of knowledge that is useful when we see patients who have had this procedure. Most of the educational material about this procedure is 5-10 years old. I look forward to hearing feedback from this group about the contemporary use of this procedure.
Previous Cases:
Missed Lung Nodule [Subscribers Only]
Radiologist expert witness writes a retrospective report that describes “asbestos-related pleural disease” on a CT abd/pelvis.
EM doctor discharges a patient with abdominal pain after reviewing a CT from 26 days earlier. She returns and is diagnosed with a duodenal perforation.
Lethal Rash [Subscribers Only]
Patient is started on allopurinol and develops a severe rash. She is transferred to a burn center, where the allopurinol is inexplicably re-started.









Too few details to know. If it was a GA case, have to wonder how he got hypoxic. However, did have one strange case of GA for septic LE amp. The guy suddenly got silent w/ mild premeds (fentanyl 1cc, lidocaine IV), so proceeded w/ induction. SpO2 fell, & intubated first attempt w/ VL. SpO2 only improved slowly, much slower than 100% O2 via ET in a usual case. Then a bradycardia. Called code, CPR, epi, etc. & proceeded with/ amputation. ROSC. Awake & talking in PACU. Pt. got a pacemaker post op. Really weird. Don't know if he had a septic embolus or what, but getting his leg off seemed to help turn the tide. If your Pt. is sick, take vigilance up a notch as it may not take much to push them over the edge. Have done more than one "sedation" w/ attempted soothing talk, no drugs, for that reason.
The convergent procedure is a epicardial afib ablation done via a subxiphoid approach. A hybrid would be doing the endocardial ablation in the same room before or after the epicardial.
They fail to state when or why the respiratory arrest occurred so it’s hard to judge. Presumably this was done under ga/ett and so it was a failure to adequately secure the airway.