A 76-year-old woman checked into the ED with pharyngitis and headache for a few days.
This occurred at the beginning of the COVID pandemic during March 2020, before widespread availability of COVID testing.
She was negative for strep.
An EKG was done for unclear reasons, and surprisingly it demonstrated a STEMI.
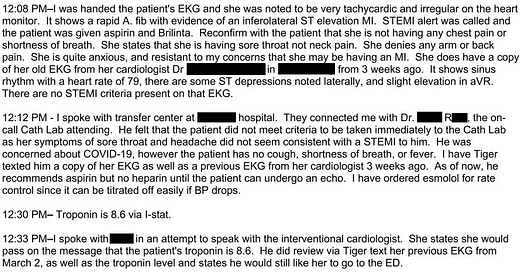
The ER doctor’s note is shown here:
Become a better doctor by reading about malpractice cases.
Subscribers get a new case every week and access to the entire archive.
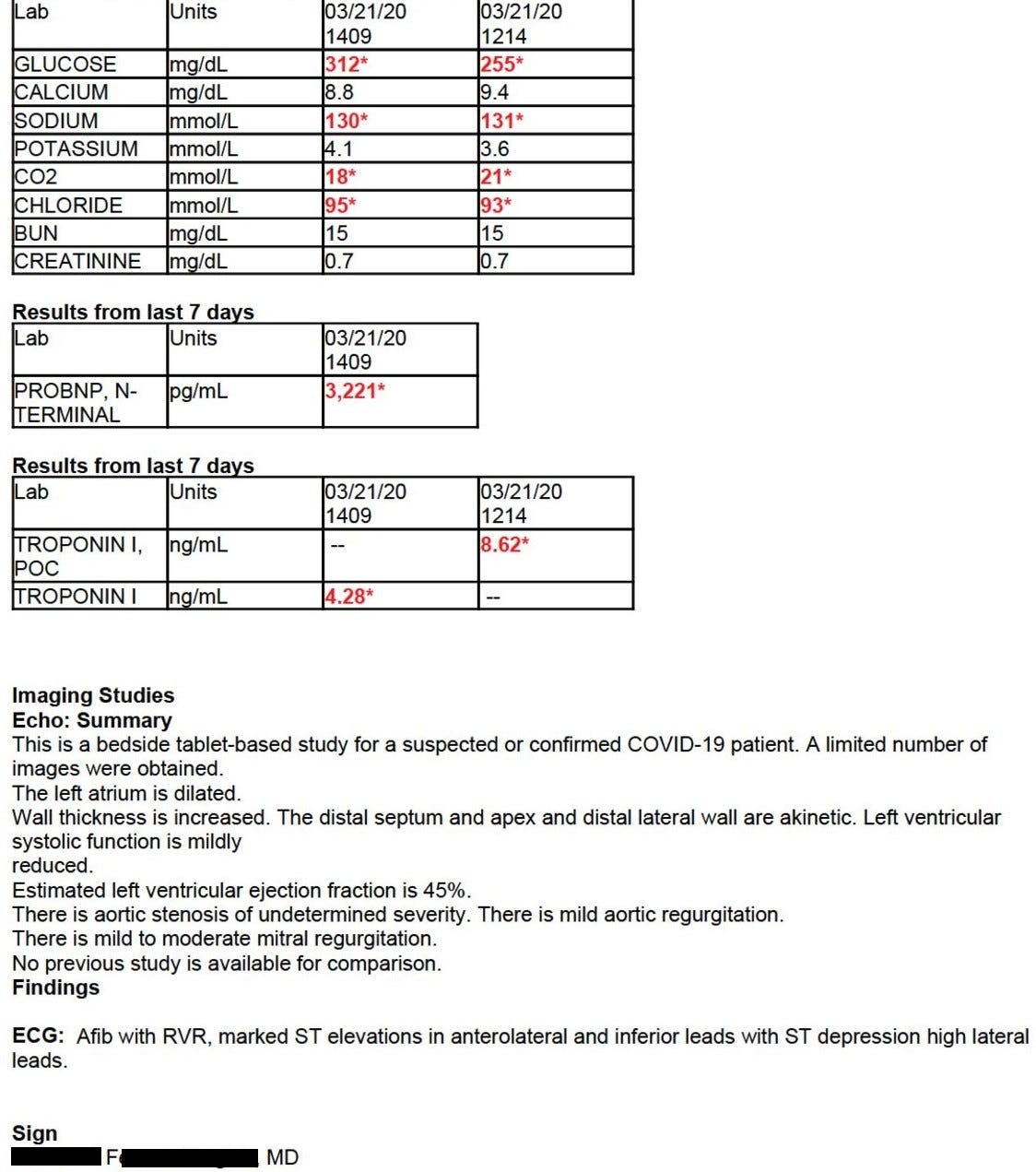
At the receiving hospital, the patient was seen by Dr. R (interventional cardiologist).
Dr. R spoke with another cardiologist (Dr. F) who was the consulting cardiologist.
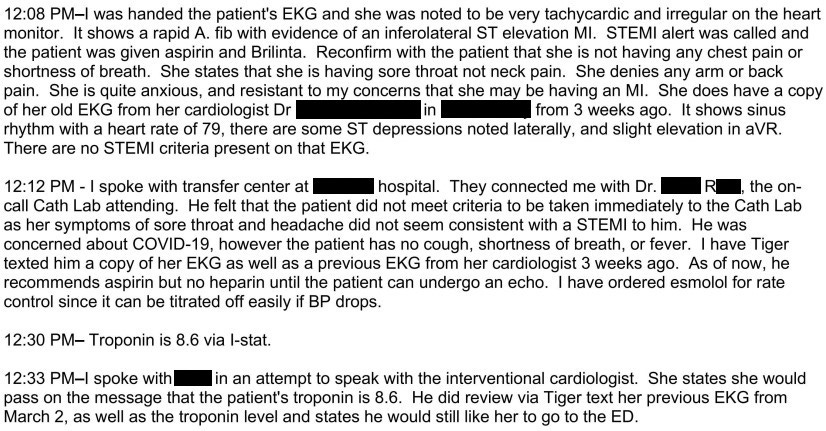
Dr. F wrote the following cardiology admitting history:
A COVID test was sent to the state lab.
The patient remained in the hospital, waiting for the result.
After 4 days of waiting, it came back negative at 7:40pm.
She was schedule to go to the cath lab the next morning.
Unfortunately she coded and died shortly before going to the cath lab.
The discharge summary is shown here:
Get CME credit for reading this case by purchasing a CME-tier subscription.
Reviewing other doctor’s malpractice cases may help you avoid your own.
Her family filed a lawsuit against multiple cardiologist who saw her and rounded on her.
The defense argued that the lawsuit should be dismissed because an executive order provided immunity for treatment related to the early days of the COVID pandemic.
The plaintiff argued that this executive order only applied to patients who were being treated for COVID.
The judge ruled and dismissed all claims against the defendants up until 7:40pm on the night before her death, when the COVID test came back negative.
The plaintiffs have continued the lawsuit, presumably on the basis that the cardiologists failed to take the patient to the cath lab at any point after 7:40pm.
They are also appealing the judge’s decision.
Join thousands of doctors and attorneys on the email list.
3 options are available: Free, Paid, and CME.
MedMalReviewer Analysis:
In order to think about this case, we need to put ourselves back into the mindset of early 2020. No one knew what was going to happen with the pandemic, and there were many unknowns about COVID. There was plausible concern that it could cause severe myocarditis or pericarditis, and PPE shortages were a very real threat. If this case were to happen today, it would be clear malpractice. But it didn’t happen today, and we need to place it in its proper context.
I’m not even sure why the patient had an EKG done during the initial ED visit. It doesn’t make sense to check an EKG on a patient with sore throat and headache. However, it’s fairly common for EKGs to be done in triage by ED techs without much thought as to why. Every ED doctor knows the misery of getting interrupted multiple times per shift to look at EKGs from the waiting room, many of which are done for no valid reason. On the flip side, the ED doctor in this case is lucky that an “unindicated” EKG was done. If it hadn’t been done, the patient would have been discharged and died at home, and the ED physician herself would have been the lone defendant. Note: As many readers pointed out, the EKG wasn’t done due to any ischemic symptoms, it was likely done due to tachycardia on the monitor as she was in a fib RVR. Thanks to everyone who was reading closely and pointed this out!
I initially was suspicious that “sore throat” was actually neck pain or jaw pain, but the ED doctor’s note indicates she clarified with the patient that she really was just describing a sore throat. On one hand, maybe we need to have a higher index of suspicion for any oral/throat/neck symptoms (I’ve seen a “dental pain” ACS presentation in an elderly patient before). But on the other hand, we simply can’t be running EKGs on every sore throat or dental pain. I think a good way to reconcile these conflicting ideas is to use age as a guiding factor. People in their 70s don’t usually come to the ED for sore throat or dental pain. I’ve published 2 other cases in which an MI was missed because of an unusual presentation, one with shoulder pain and one with upper back pain.
The key factor that supports the cardiologist’s plan to defer catheterization is that she had no chest pain, shortness of breath, or other symptoms of acute coronary syndrome. We always need to correlate a patient’s test results with their clinical presentation, and it’s debatable if the clinical presentation in this case mandated urgent catheterization. Rushing people to the cath lab is not without risk, as illustrated in this previous case I published titled “STEMI Cath Perforates Coronary Artery”. However, the EKG findings, wall motion abnormalities, and rising troponin totally change the assessment.
Despite a lack of chest pain and the possibility that she might have viral myocarditis, it’s clear that the cardiologists thought she should have a catheterization done. The COVID test result was not going to change whether or not she needed a catheterization. The only thing it changed was whether or not they were going to wear PPE. I understand not wanting to waste PPE, but I think the legitimate potential for potentially-fatal disease outweighs that concern.
I really wish they would have done an autopsy. My suspicion is that she did truly have acute coronary syndrome, but I think there is a very reasonable possibility that she had myocarditis from a non-COVID viral etiology. It’s interesting that the patient was noted to be in PEA during the code. The patient was found down in her room, and there’s a possibility that she was actually in V fib or V tach prior to PEA.
Society’s collective lack of preparedness for pandemics (that were long telegraphed by SARS and MERS) not only meant that many patients died of COVID, but our response also resulted in collateral damage that killed many non-COVID patients like this one. I can think of 2 take-home points about how we can prepare for future pandemics to avoid these outcomes:
Stock-piling PPE. Having adequate PPE probably would have saved this patient’s life.
Preparing every hospital to run PCR tests locally for novel infectious agents. We should have a national plan to manufacture and distribute primers against new threats at breakneck speed. The genetic sequence of many of these microbes is known within a few days of discovery, and this information can be used to make the necessary reagents before the threat is even at our borders. Widespread availability of fast and local PCR testing could have saved this patient’s life.
A note for CME subscribers: You will receive a course evaluation on February 28 to claim your credit for this case and all February 2025 cases.









When I was an intern early on in the Covid pandemic, the same thing happened at my hospital - cardiologists refused to take pts to the cath lab. It was okay for the ER doctors to go into the patients room, but god forbid the sacred cardiologist has to stand at the patients groin to do a procedure.
It’s a very real possibility that this was a falsely negative Covid PCR as well (it’s not well remembered how poorly sensitive the initial tests were, esp nasal swabs). Interpreting this case really requires knowledge of the locale (eg high prevalence such as NYC or somewhere like AZ)