What other physicians are saying about The Expert Witness Newsletter:
"Reading your material has definitely shaped my documentation & my approach to the undifferentiated patient." - Dr. Emily Hamburg-Shields
A 65-year-old man presented to a pain management clinic for low back pain. He was seen by Dr. F, who is a board certified anesthesiologist and pain management physician. He underwent an uneventful lumbar epidural steroid injection. Four days later he developed fever, weakness and confusion. He was found to have a brain abscess and severe hydrocephalus. He was transferred to an academic medical center, where an EVD was placed with frank purulent discharge. He died several days later.
A lawsuit was filed alleging that the physician was negligent in his antiseptic technique. He had used Betadine, and the plaintiffs felt that Chlorhexidine should have been used instead. The allegations of negligence are shown here:
The expert witness opinion is shown here:

The lawsuit was withdrawn 4 months after it was filed; a confidential settlement was reached.
Join 4600+ other physicians who are becoming better clinicians by reviewing cases that you won’t find anywhere else.
MedMalReviewer Opinion:
1) This case is a good opportunity to review the literature comparing Betadine and Chlorhexadine for epidural injections prior to reading this case. While epidural steroid injections are usually done only by specialists, there is a reasonable argument that the same literature should be strongly considered by any physician performing lumbar punctures. This link has a good review of what is known about the subject, highlighted by the excerpt below.
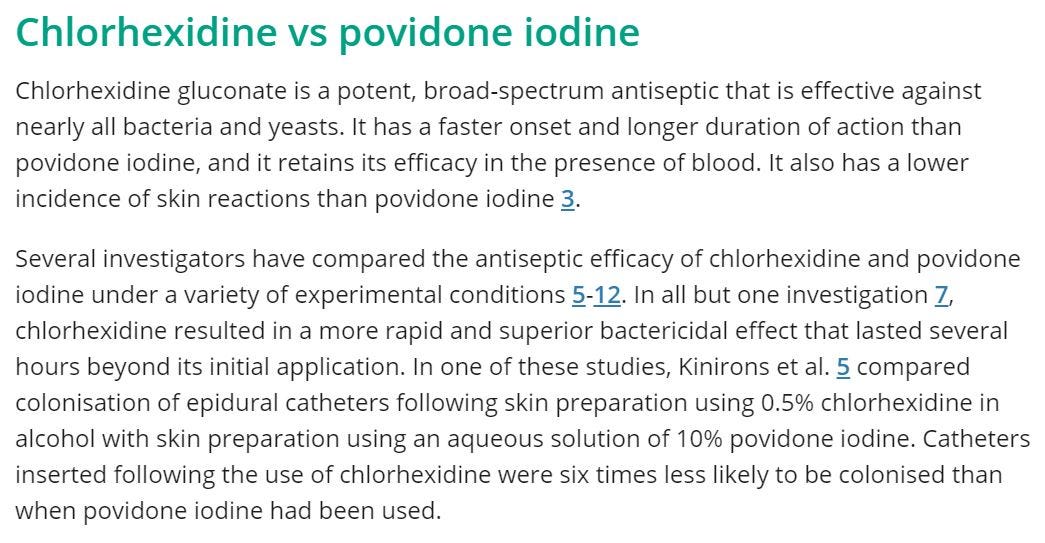
2) However, the chlorhexidine label specifically says it should not be used in any situation where it may contact the meninges. A short letter to the editor discussing this is available here.
3) Both the physician and the hospital were sued. Hospital policies are usually used as evidence that the physician did not follow the standard of care at their own facility. However this case demonstrates a rare situation in which the physician followed their hospital protocols and still was accused of negligence.
4) Rapidly reaching a settlement is the wise move here. There was a devastating outcome that was clearly related to the procedure. Even if the physician can make a reasonable argument that he was following his own hospital protocols, the risk of a sympathetic jury and massive settlement is too great in our current medicolegal environment.
Check out the 3 most recent cases:
Case #22: Ureter Injury [Subscriber Content]
Specialty: Neurosurgery
Synopsis: Patient undergoes L3/L4 fusion, discharged, comes back with abdominal pain and wound drainage. Extensive urologic repair required for transected ureter.
Specialties: EM, Psychiatry
Synopsis: Patient seen in ED after trying to jump out of a moving car. Seen by ED physician and psychiatry social worker, discharged, dies by suicide 5 hours later.
Case #20: Wrong-Site Surgery [Subscriber Content]
Specialty: General Surgery
Synopsis: Patient elects to have a large lipoma removed from his back, surgeon allegedly removes a completely different and smaller lipoma.



No wonder it was settled and not taken to trial. On one hand, a bad and sad outcome for Pt. On other hand, the plaintiff side is arguing that the physician should have willingly gone against an explicit statement in the CHG package insert. I cannot reconcile this as in our practice we use betadine for ESI and LP given the CHG package insert statement.
What exactly does it mean when a settlement is reached? Does that mean that the patient's family and the hospital negotiated a dollar amount as compensation for the patient's death?
I don't quite understand. What was the malpractice?