An elderly woman presented to the ED with back pain.
After workup she was started on Bactrim for presumed UTI/pyelonephritis.
She returned to the ED 2 days later with swelling and redness in her eyes.
Eye drops were prescribed and she was discharged.
She had 2 more bounceback visits, until she was admitted to the hospital and diagnosed with Stevens-Johnson Syndrome.
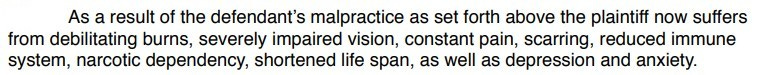
The patient survived but suffered long-term debility as described here by the plaintiff’s attorney:
Become a better doctor by reviewing malpractice cases.
The plaintiff sued the hospital alone.
The ER doctor was not named as a defendant.
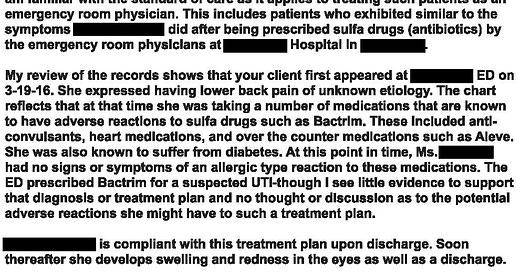
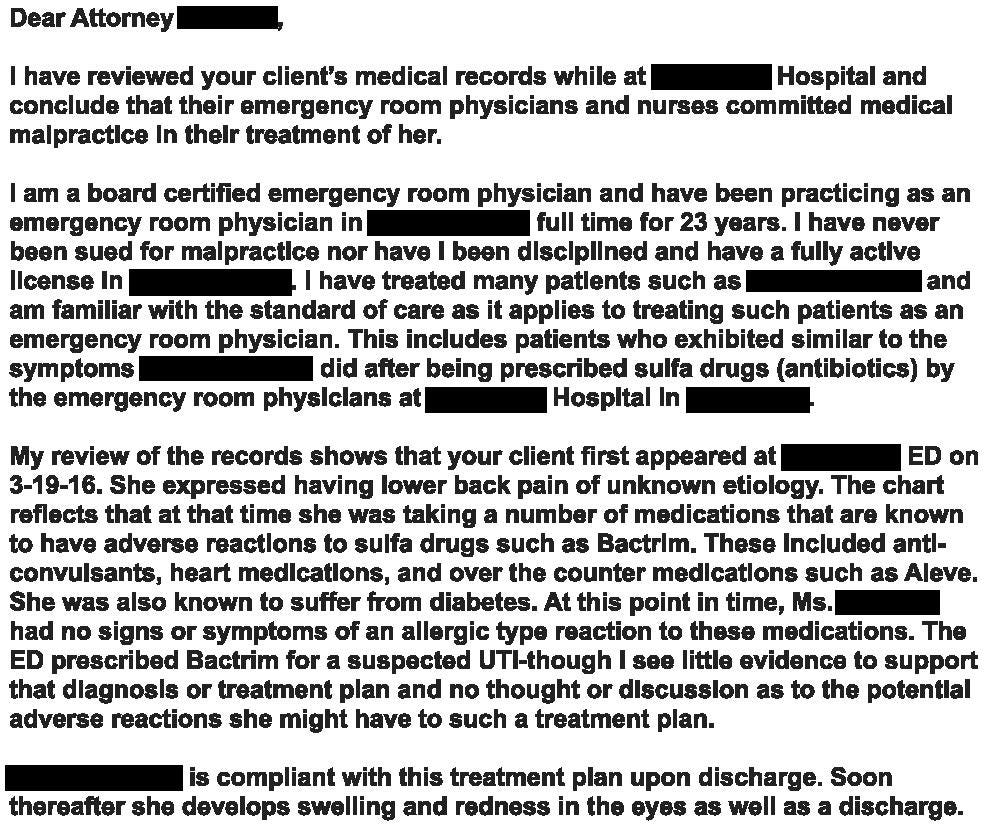
The expert witness opinion is shown here:
They offered to settle with the hospital for $995,000.
The lawsuit was settled before trial.
Paying subscribers get a new case every week and access to the entire archive.
CME subscribers get 12 credit hours per year.
MedMalReviewer Analysis:
The expert opinion was poorly written. There are several typos and numerous unaddressed issues. The expert calls into question the initial diagnosis of UTI, but does not provide any clarification about what workup was done. If the patient had no urinary symptoms and there were no UA or urine culture findings to support a UTI diagnosis, then a key issue here was the decision to start antibiotics (regardless of which antibiotic was selected).
Despite the poor expert opinion, there are still some valuable learning points in this case. The most interesting thing I found was this study in which 42% of SJS patients experienced conjunctivitis before the onset of skin eruption. These patients also had better vision outcomes when started on ocular steroids. This is a good reminder to think about SJS when seeing patients with conjunctivitis.
The expert claimed that the diagnosis “should have been obvious”, which I absolutely disagree with. The initial symptoms are usually vague and non-specific, which makes diagnosis nearly impossible for the first few days. Per the study cited above, fever, malaise and sore throat are the most common presenting symptoms. Medical educators focus primarily on skin findings in the diagnosis of SJS. In some ways this is appropriate because the rash is really what helps us narrow the diagnosis, but in some ways this is a disservice because the rash is a delayed finding. Patients who present with vague malaise and fever are challenging because they usually just have a virus, but sometimes you miss meningitis or SJS or bacteremia or any other number of diagnoses that are certainly not “obvious” and just need extra time to declare themselves.
I’ve covered one SJS case previously (fair warning, its a paywall case), which was caused by allopurinol. Between these 2 cases we’ve hit the 4 most common medication categories that can cause SJS:
Antibiotics (Bactrim in this case)
Allopurinol (especially doses >200mg as occurred in the previous case)
Anticonvulsants (patient in today’s case was on them)
NSAIDs (patient in today’s case was on Aleve)




Drives me crazy how the so-called expert witness keeps saying an adverse reaction is an "allergic reaction"...
Thank you, med mail reviewer for an excellent critique and for all of the insightful and honest comments. I will probably never look at a case of conjunctivitis quite the same way again.