An 88-year-old woman presented to the ED with 9 days of coughing.
She lived in Mexico but was just a few miles from the border, so she came to the US for her medical care.
She was a Jehovah’s Witness and had been on warfarin for 20+ years due to a bioprosthetic valve and atrial fibrillation.
CBC and CMP were unremarkable.
Troponin was slightly elevated at 0.06.
Flu test was negative.
CXR was reassuring.
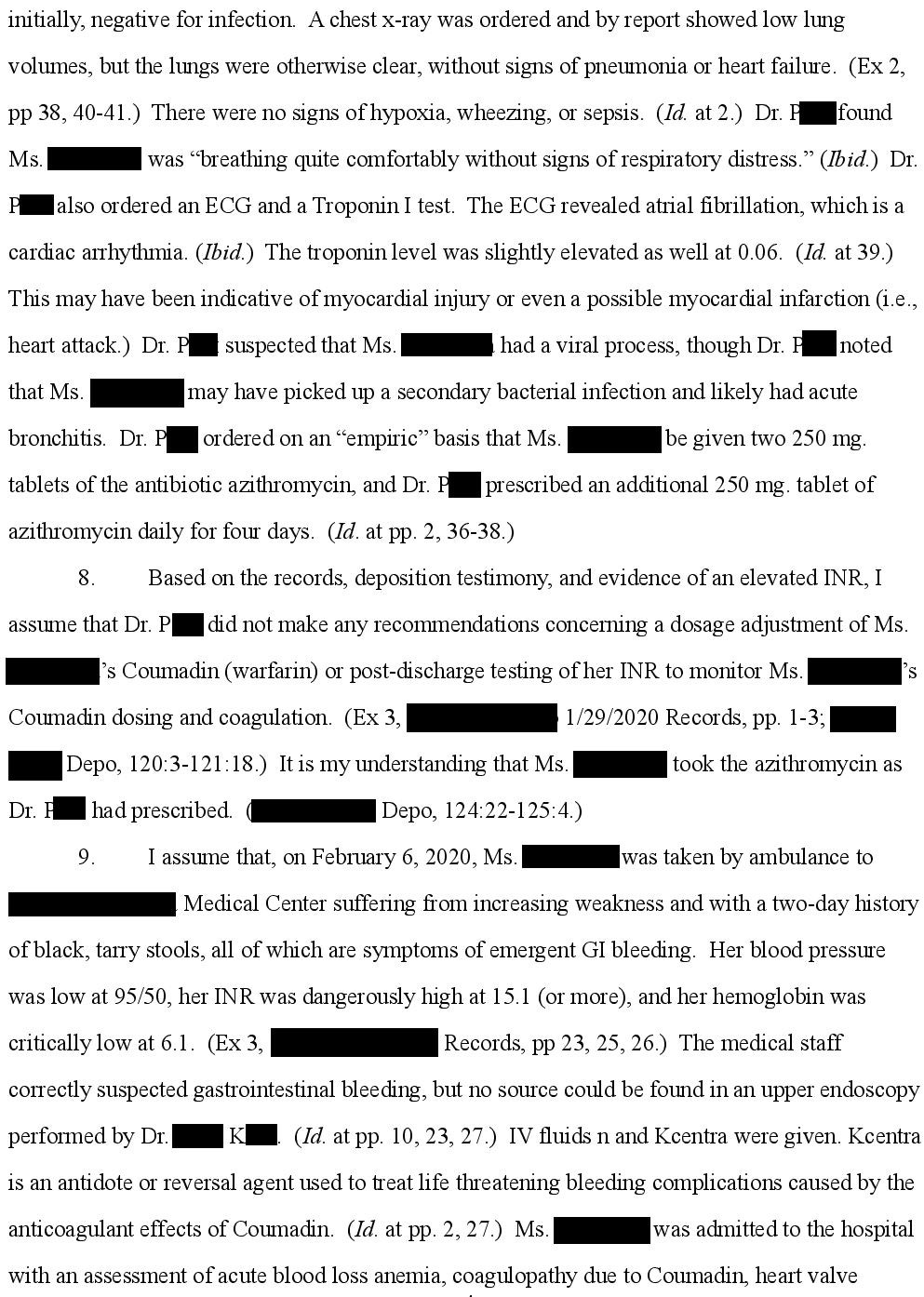
INR was slightly supratherapeutic at 3.9 (target range 2.5 - 3.5).
The ED physician (Dr. P) was worried about a bacterial infection superimposed on a viral illness.
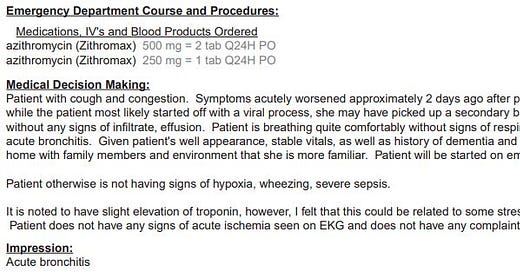
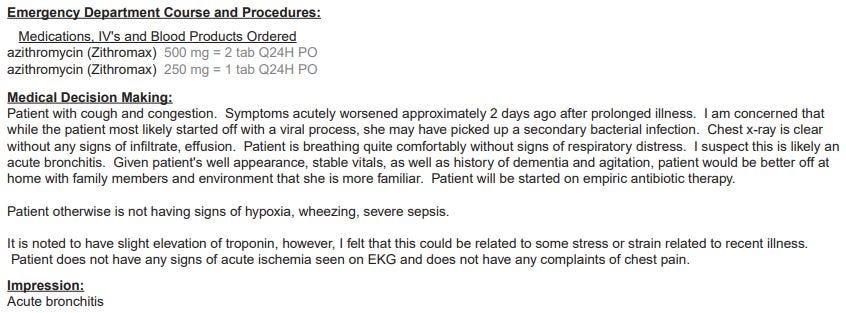
She ordered azithromycin 500mg PO in the ED, and sent a prescription for 250mg qday x 4 days.
The patient was discharged.
The physician’s impression is shown below:
Join 16,000+ doctors and attorneys on the email list.
Free and paid options available.
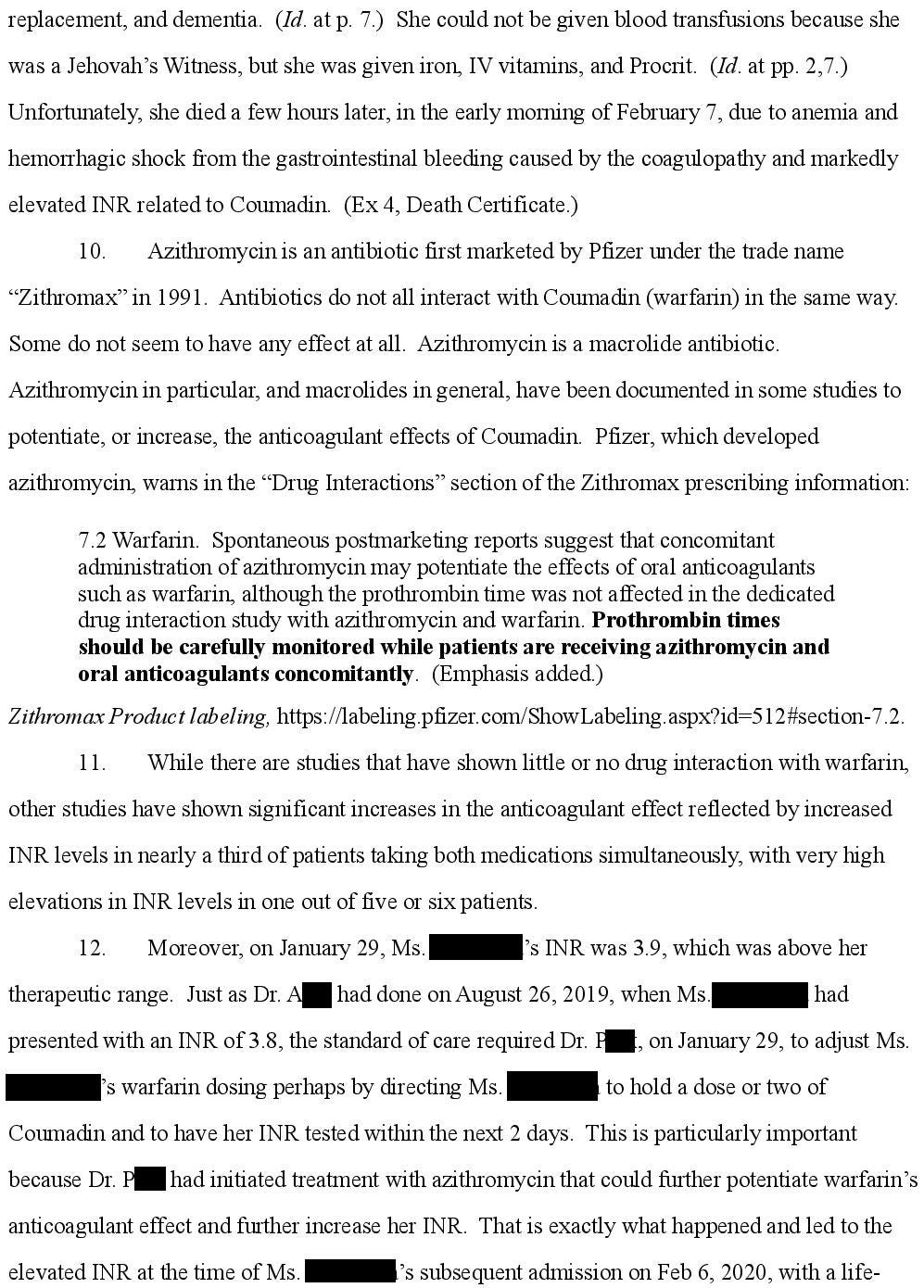
The patient returned to the ED 8 days later.
She was very weak and had 2 days of black stools.
Her INR was >15, hemoglobin was 6.1, and she was hypotensive.
She was given KCentra and fluids, and admitted to the ICU.
An EGD was done but no source of bleeding was identified.
She was given iron infusions, vitamin K, Procrit, and a PPI.
The family refused any blood products in keeping with their Jehovah’s Witness faith.
She died the following day of complications from the GI bleed.
The family sued the ER doctor.
They allege that the azithromycin caused her INR to rise, resulting in her death.
The plaintiff’s expert opinion is shown below.
Note that point 5 discusses a previous ED visit in 2019, before getting to the ED visit in 2020 that led to this malpractice case.
Become a medicolegal expert by reviewing a new case every week.
Learning from a wide variety of lawsuits will help you be a better doctor.
The defense hired an EM physician:
Settlement negotiations were unsuccessful.
The lawsuit went to a jury trial.
At trial, the patient’s family testified that the physician spoke with them about the elevated INR, but they did not ever recheck it on their home device or take her to the coagulation clinic.
The jury returned a verdict for the defendant:
Following the trial, the defendant reported the plaintiff’s expert to ACEP for unethical testimony.
In his deposition, he admitted that the only literature he reviewed was given to him by the plaintiff’s attorney.
He also admitted that after writing an initial opinion, the plaintiff’s attorney asked him to make several edits, which he did.
The expert had retired and was no longer an ACEP member.
Therefore the case was not reviewed further by ACEP and no censure was issued.
MedMalReviewer Analysis:
There is controversy about the significance of the interaction between azithromycin and warfarin. It didn’t make it on The Official Warfarin Drug Interaction List (one of my favorite articles about the topic). A study of VA patients found that azithromycin caused significant INR elevations but did not result in any serious bleeding complications. I don’t think this doctor fell below the standard of care, but this case is a good reminder to tell patients to closely monitor their INR when starting new medications that have the potential for a drug interaction.
Patients have the right to decline treatment for religious reasons even if it seems foolish to the medical community and ultimately kills them. However, I don’t think they should be able to sue if their refusal of critical medical interventions is a major contributing factor to their death. In my experience, local Jehovah’s Witness congregations often have medical liaisons that can help navigate these sensitive issues. Filing questionable malpractice lawsuits only serves to anger physicians. This is an unwise decision coming from a member of a community that requests special treatment and already places additional stress on doctors.
Issues related to anticoagulation are the most common type of malpractice case that I see. Every specialty has a few unique malpractice themes, but anticoagulation-related lawsuits unite us all, from generalists to specialists, medical doctors and surgeons. Here are some previous cases I’ve covered:










Good case. The plaintiff expert made a lot of comments that were very questionable. Not only did he not rely on reliable literature in the subject, but he made a point to say the physician should have been overly cautious because of the patient's faith. This was strange considering that this visit was completely unrelated to GIB and her use of coumadin, and ER doc is not the one who chose to put an 88 yo woman with dementia and anti blood beliefs on coumadin. I also find it unlikely that her faith came up since patient wasn't even able to provide any meaningful history due to her underlying dementia. This was a weak case at best, but it is concerning an "expert" would manipulate the literature and/or only look at one study in order to make the lawyer happy.
My takeaway: be very careful with anticoagulation. Document discussions and risks/benefits.