A 49-year-old man presented to the ED with chest pain that had been present for several hours.
He also reported “GI upset” and “feeling winded”.
A troponin I was ordered and was within normal limits.
A d-dimer was also within normal limits.
The chest x-ray was interpreted as “no acute cardiopulmonary findings”.
The EKG was interpreted as normal but unfortunately was not included in the court documents.
The physician documented a differential diagnosis including “AMI, CHF/pulmonary edema, costochondritis, hyperventilation, musculoskeletal pain”.
The patient was given a GI cocktail.
He was discharged at 4:12am, just under 3 hours after presentation.
The discharge instructions were to follow-up the next business day, or “return to the ED if the chest pain returned”.
At 5:58am, the patient returned by ambulance in cardiac arrest.
He had been found unresponsive in his car.
Despite 30 minutes of resuscitative efforts, he died.
Become a better doctor.
Subscribe today to learn from lawsuits your colleagues have faced.
The patient’s wife and minor children contacted a law firm.
A lawsuit was filed against the physician, the EM group, and the hospital.
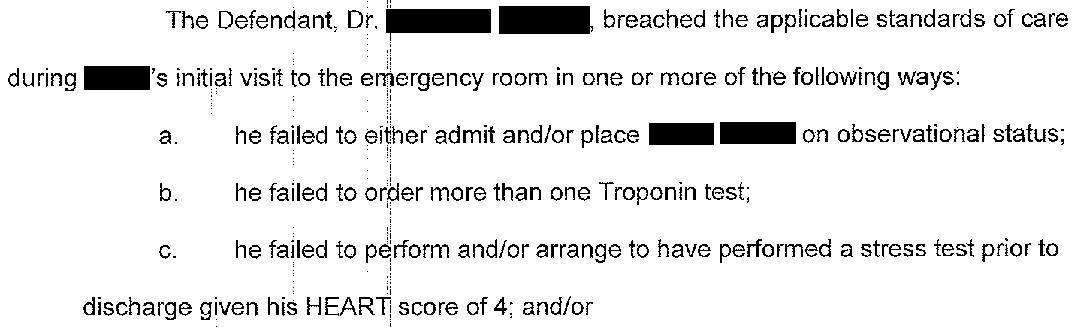
They made these specific criticisms:
The physician in this case is an academic med/peds faculty member who was working in a community ED.
The initial plaintiff expert was written by an EM/IM physician. It is very brief but was included to establish an expert with similar training as the defendant.
A 2nd plaintiff opinion was written by an EM doctor:
The same EM expert made further clarifications to her criticisms of the defendant:
A cardiology expert was also hired by the plaintiff:
The defense disclosed their own EM expert:
The plaintiff offered to settle.
From the hospital, they requested:
$3,000,000 for the widow
$250,000 for the child
From the EM group, they requested:
$1,000,000 for the widow
$250,000 for the child
From the doctor, they requested:
$1,000,000 for the widow
$250,000 for the child
A confidential settlement was reached and the lawsuit was withdrawn.
Become a medicolegal expert.
Subscribe today to get a new case every week and access to the entire archive.
MedMalReviewer Analysis:
This lawsuit focused primarily on the importance of the HEART score, which reportedly was 4 (exact scoring not described). The plaintiffs claim that all scores of 4 or higher should be admitted, but I don’t agree with that claim. This practice used to be more common, but now most hospitals and cardiology departments are really trying to push people home and get outpatient stress tests instead. Part of me wants to argue that its impractical to admit every chest pain and that the push to discharge patients over the past few years is warranted. Another part of me wants to point out that hospitals are refusing to admit chest pain for purely financial reasons and that these policies are unfairly causing blame to be placed solely on the ED physician when the inevitable bad outcome happens.
Another key criticism was the fact that only one troponin was checked. I couldn’t figure out why the doctor didn’t wait for the 2nd troponin, until I read the defense opinion and it became clear that the patient had been having chest pain for many hours prior to presentation. This is a common scenario I face in the ED. No one wants to waste time waiting for a repeat troponin when the waiting room is full and a patient has already been having chest pain for more than 3 hours at the initial troponin check. After having reviewed a number of MI malpractice cases, my practice has changed and I am much more likely to wait for a repeat troponin regardless of how long a patient says their chest pain has been present.
I’m glad an autopsy was done, because it rules out the other common possibilities such as dissection or PE. However, I’m a bit concerned that neither side discussed the autopsy in more detail. If this was truly an MI, there should have been histological evidence. The defense claims that the patient died of a fatal arrhythmia. This is either a disingenuous way of admitting that the patient died of an MI (V fib or V tach), or could be a signal that nothing was found at autopsy to explain the patient’s death (as can happen with some isolated arrhythmias).
I’ve covered a few other missed MI cases. All 3 resulted in the patient’s death.
One was challenging because it presented as musculoskeletal shoulder pain.
Another was challenging because it presented as upper back pain.
In the OMI case I published, the patient presented with chest pain but only had one troponin done (just like this case).






where i trained, the heart score was followed pretty closely. this guy would have been admitted most likely. where im at right now, heart score of 4 with 2x neg trops and assuming the EKG was read correctly and was actually stone cold NSR, this would have been a tough sell to IM to admit and i know my colleagues would likely dc this.
I practiced in a community emergency department about 45,000 visits or less. I’ve been using the hard score and now favor the heart pathway score when evaluating adults with chest pain. Depending on the score you can use the regular heart score which seems to favor discharge versus the heart pathway and that when it’s for higher, they recommend observation and further evaluation. When I calculate the heart score pathway score on MDCalc there’s a function if you get yourself registered for free you can cut and paste it which I do into the EMR. Then quickly dictate a reason if the patient’s heart score is four or higher that either recommended admission or we discussed the risk and benefits, and the patient made the decision with medical decision capacity to go home watch for the following signs and symptoms and ensure appropriate follow up.