A 63-year-old man slipped and fell on ice while walking out of Dunkin Donuts.
He injured his right knee and was taken to the ED.
X-rays did not show any fractures.
He was referred to see ortho as an outpatient.
The patient followed-up with his PCP (Dr. C) who repeated x-rays and a DVT US, both of which were negative.
He also saw several orthopedic surgeons, and was ultimately diagnosed with a tear of his quadriceps tendon.
Dr. F (orthopedic surgeon) recommended surgical repair and requested labs and clearance from the patient’s PCP.
Dr. C cleared the patient for surgery but wrote in his note “I believe he represents significant risk for post-operative thrombophlebitis”.
The surgery was uncomplicated.
3 weeks after the surgery, the patient developed sudden dizziness and shortness of breath.
He coded in the ambulance on the way to the hospital.
Autopsy confirmed DVT and pulmonary embolism.
Become a better doctor.
Review a new malpractice case every week.
The patient’s family sued the orthopedic surgeon and the hospital.
The plaintiff offered to settle for $2,400,000.
The defense rejected this offer.
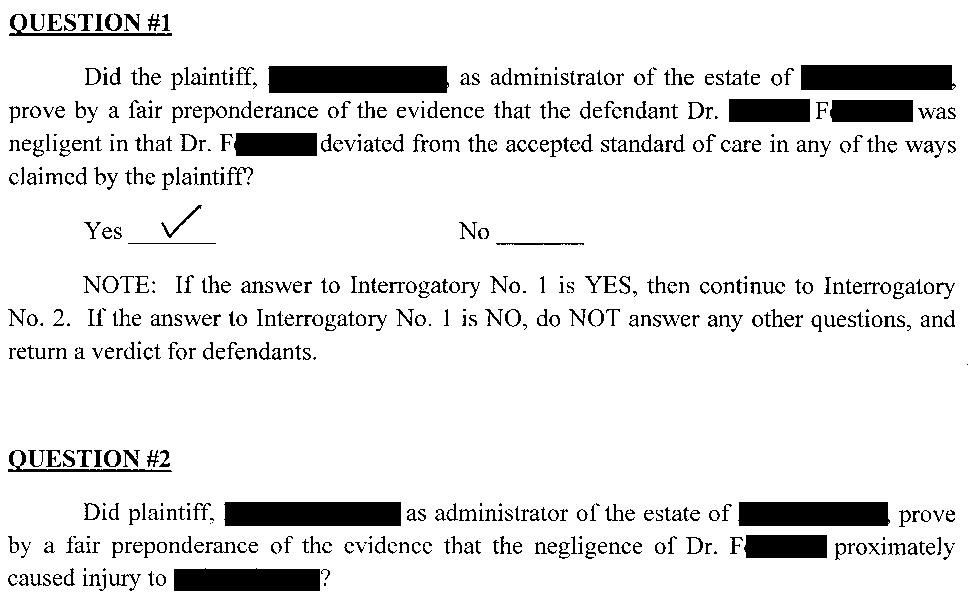
The jury returned a verdict for the plaintiff for $12,500,000.
Protect yourself from lawsuits.
Subscribers gain insight into common plaintiff legal tactics and sharpen their medical knowledge.
MedMalReviewer Analysis:
There’s no other way to put it, this is a terrible outcome for the orthopedic surgeon. His malpractice insurance probably covers a million of this, maybe 2 or 3 million if he is lucky. But no individual physician has limits anywhere close to $12,500,000. A lot of people always email me and ask what happens if you lose a verdict far above your liability limits, and there’s not always one clear answer. If the hospital is also a defendant, their (much larger) policy might kick in. There’s a chance the physician could file a “bad faith” claim against his own insurance company, if they gave him bad advice or pushed him to go to trial despite his request to settle. This case is a perfect example of why you might want to settle even if you are absolutely certain you didn’t do anything wrong. It doesn’t feel good to turn down a $2,400,000 settlement offer and then lose this badly.
The PCP’s note mentioned “significant risk for post-operative thrombophlebitis”, but that’s not a very helpful statement. Everyone knows there’s always significant risk of thromboembolic disease after a surgery. It doesn’t seem to indicate any specific risk stratification (high/medium/low) or percentage risk that could be referenced to any literature or translate to an actionable decision. The PCP didn’t recommend any particular approach to reducing this risk.
I’m a bit surprised the PCP didn’t get named in the lawsuit too. The plaintiffs could have easily accused him of not providing specific anticoagulation recommendations and not providing education about DVT/PE. From the looks of it, the jury probably would have thrown at least a few more million onto the verdict if they were given the opportunity.
I’ve covered a few other pre-surgical “clearance” lawsuits, and the striking thing is that they all involve extremely poor communication between the PCP and the surgeon. The miscommunication wasn’t actually the causative issue in all of these, but the attorneys certainly will use it to make you look dumb and sloppy.
Orthopedic surgeon does an EKG at a pre-op visit allegedly showing ST changes, but never sends it to the PCP, who clears the patient without doing his own EKG. Patient dies of MI shortly after surgery.
Colorectal surgeon tells his patient to talk to his PCP about stopping his warfarin before genital wart surgery, but never communicates with their PCP or checks to see if the patient actually did. Patient has a large stroke (but was probably unrelated to his anticoagulation).
Bariatric surgeon tells patient to talk to PCP about prolonged aPTT prior to surgery, which doesn’t happen and no one follows-up. Patient has bleeding complications and stroke.
This case also hits on another key theme I’ve learned from writing this newsletter, which is that coagulation topics are the most common malpractice topic I see. There are tons of examples including DVTs, pulmonary emboli, arterial extremity clots, thromboembolic strokes, warfarin dispensing errors, drug interactions, spleen lacerations, hemorrhagic shock after trauma, failure to monitor Xa levels, and many more. These topics affect nearly every specialty and any decision-making related to bleeding or coagulation should be considered high risk.






Maybe I’m not up to date on the latest and greatest anticoagulation guidelines, but per the 2012 CHEST guidelines for isolated lower extremity injuries requiring immobilization (quad rupture would seemingly fit this) they recommend no thromboprophylaxis. Not to mention this patient was WBAT after surgery. It’s kind of like, why even consider the guidelines and not just anticoagulate everyone for every surgery if you can just get sued anytime someone gets a DVT/PE.
The term thrombophlebitis, which is not a life threatening condition, is being incorrectly here. The PCP meant thrombosis or thromboembolism.
In any case, medically this hinges on whether the standard of care in 2015 required post operative blood thinners. I’m not aware of any evidence that it did.
I guess it would have helped the orthopedic surgeons defense if he documented a discussion of risks and benefits of post operative blood thinners, but I still can’t see how he did anything wrong. I wonder if there’s any grounds for appeal here.